Nevada’s informed consent medical malpractice case law balances statutory protection for healthcare providers with evidentiary standards defining what consent-related evidence reaches juries.
Recent rulings under Nevada’s Revised Statutes (NRS) §41A.110 have reshaped how defense counsel present consent documentation and when such evidence is admissible at trial.
These developments require both plaintiff and defense attorneys to reassess long-standing strategies. Effective case preparation now hinges on aligning consent documentation, standard-of-care determinations, and assumption-of-risk defenses within Nevada’s evolving malpractice framework.
Nevada's Statutory Foundation for Informed Consent
Nevada’s informed consent framework combines statutory conclusive-consent provisions with common-law evidentiary principles. NRS 41A.110 defines the elements required for conclusive consent and specifies that noncompliance “does not of itself constitute negligence.”
Conclusive Consent Requirements Under NRS 41A.110
To obtain statutory protection, providers must:
- Explain the procedure in general terms
- Discuss alternative treatments or procedures
- Describe the general risks involved
- Obtain the patient’s signed acknowledgment containing these explanations
In Allan v. Levy (1993), the Nevada Supreme Court held that missing any element voids conclusive-consent status.
The statute functions as a defensive shield, not an affirmative duty. Compliance bars further inquiry into disclosure adequacy, but failure to meet all elements does not create automatic liability.
Professional Standard Application Across Healthcare Providers
In Bronneke v. Rutherford (2004), the Court applied the professional-standard test across licensed providers, including chiropractors, and rejected a patient-oriented approach.
Breach must be proven through expert testimony showing what a reasonable practitioner in the same specialty would disclose, maintaining Nevada’s alignment with a professional, not patient, standard.
Integration with Medical Malpractice Framework
Informed consent claims operate within Nevada’s overall malpractice scheme under NRS Chapter 41A and NRS 41A.100(1), which require expert proof of breach, causation, and damages.
Conclusive consent under §110 offers limited statutory protection but does not excuse a provider from the underlying duty to meet accepted standards of care.
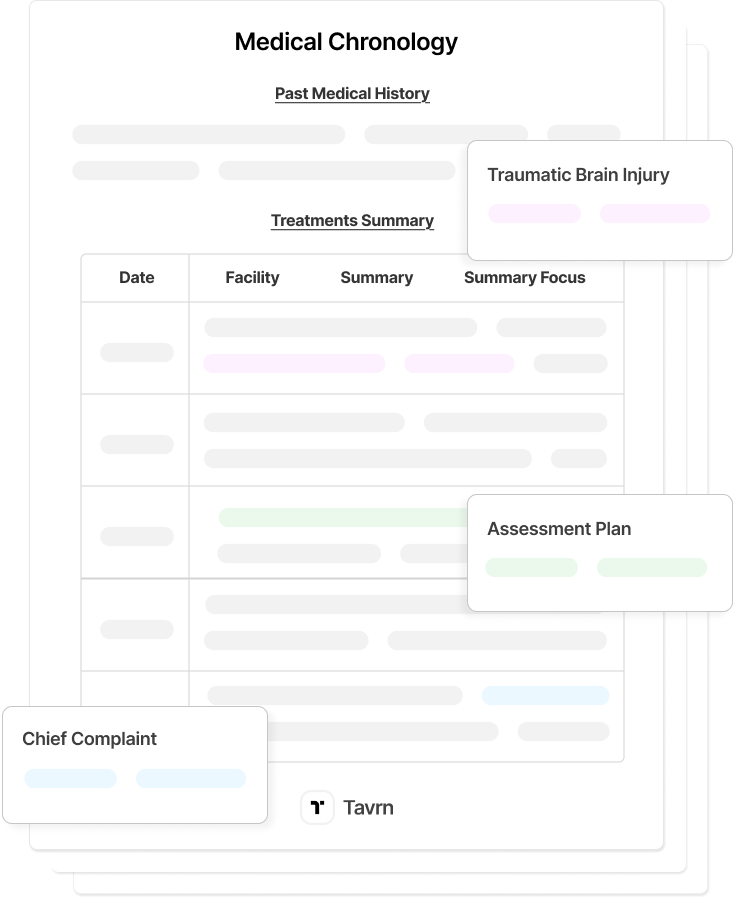
Illustrative Case Analysis: Consent Evidence Limitations
A representative surgical malpractice case demonstrates how evidentiary restrictions on consent documentation shape admissibility arguments under Nevada law.
The practical implications of Nevada's consent evidence standards emerge in medical malpractice cases in which plaintiffs focus exclusively on standard-of-care violations without challenging the validity of consent. Such decisions alter trial dynamics and available evidence for both parties.
Hypothetical Case Background and Proceedings
In this scenario, a patient undergoes an anterior cervical discectomy and fusion for chronic neck pain and radiculopathy, later developing permanent vocal cord paralysis and swallowing impairment. The plaintiff sues for negligent surgical performance but does not contest informed consent, focusing solely on intraoperative violations of the standard of care.
Defense counsel moves to admit the signed consent form acknowledging vocal cord injury risks. The motion becomes central to pretrial evidentiary disputes over whether the consent document is relevant when consent validity is not challenged.
Trial Strategy Under Evidentiary Limitations
At trial, the motion faces scrutiny under Nevada’s relevance standards. Because consent validity is uncontested, the court limits admission of the consent form, requiring the defense to rely instead on expert testimony regarding surgical technique, complication rates, and accepted practices.
Plaintiff experts testify that the surgeon deviated from standard visualization techniques, while defense experts describe recognized complication risks and procedural norms.
The evidentiary restriction prevents the defense from using consent documentation as a proxy for compliance with the standard of care.
Strategic Implications for Practice
This scenario illustrates how evidentiary constraints reshape malpractice strategy. When consent validity is uncontested, defense counsel cannot depend on consent documentation as a central defense, increasing reliance on expert testimony and alternative causation theories.
For plaintiffs, the same limitations remove a traditional defensive tool and narrow the case to breach and causation. The decision to challenge, or preserve, consent validity becomes a pivotal strategic factor influencing case development and settlement posture.
Evidentiary Standards for Consent-Related Evidence in Nevada
Nevada courts apply strict relevance analysis under NRS 48.035(1), admitting consent-related evidence only when it directly relates to disputed issues. This narrows traditional defense strategies and distinguishes expert medical testimony on procedural risks from lay testimony about consent discussions.
Evidence Admissibility When Consent Uncontested
When plaintiffs do not dispute the consent process, consent forms, discharge instructions, or risk acknowledgments are often excluded as irrelevant to professional negligence claims.
Courts reason that such materials do not make negligence “more or less probable” under Nevada’s malpractice framework.
This distinction separates consent validity, which is focused on patient authorization, from standard-of-care compliance, which governs how treatment is delivered. Evidence pertinent to one issue may be inadmissible for the other, limiting defendants’ ability to rely on consent documentation when consent itself is not challenged.
Expert Testimony Distinctions
Expert medical testimony remains admissible when it assists the jury in evaluating breach and causation. Experts may describe recognized procedural risks or complication rates only if those opinions clarify standard-of-care questions rather than assumption-of-risk defenses.
Establishing this connection requires careful foundation laying to show that risk testimony relates to negligence, not consent.
Strategic Decision Point for Consent Challenges
Nevada’s evidentiary approach creates a pivotal tactical choice for plaintiffs: challenging consent opens the door to assumption-of-risk defenses, while preserving consent validity may bar the defense from introducing consent evidence entirely.
Plaintiffs must balance the benefits of asserting inadequate disclosure against the risk of allowing the jury to hear risk acknowledgments.
Foundational Precedents and Evolving Standards
Nevada’s informed consent jurisprudence rests on two core precedents, Allan v. Levy and Bronneke v. Rutherford. Together, these precedents define statutory compliance and professional disclosure standards, continuing to shape evidentiary rulings and case strategy under modern relevance analysis.
Allan v. Levy Summary
In January 1984, plaintiff Linda Allan injured her back at work and was referred to neurosurgeon Dr. Levy, who scheduled a lumbar laminectomy. The night before surgery, Allan indicated she wanted to review her test results before consenting. After being given sedatives and undergoing a late-night phone call with Dr. Levy, she signed a standard hospital consent form. A surgical complication followed, leading Allan to sue for lack of informed consent.
At trial, a jury returned a defense verdict. On appeal, the Nevada Supreme Court evaluated the consent form under NRS 41A.110’s conclusive‐consent framework, finding that although compliance with the statute is not required for liability, the four statutory elements must all be present for “conclusive consent” protection. Because the form did not explain alternatives or general risks, the “conclusive consent” jury instruction given at trial was erroneous.
The Allan decision holds that Nevada’s conclusive‐consent safe harbor will not apply unless all elements of NRS 41A.110 appear in the consent documentation. Even a signed form that omits required elements may allow a jury to examine disclosure adequacy.
For practitioners, the case emphasizes that generic forms may fail to secure the safe harbor, and that expert testimony and consent-process documentation must closely align with the statute.
Bronneke v. Rutherford Summar
In June 2001, plaintiff William Bronneke sought treatment from chiropractor Dr. Rutherford for chronic neck and back pain. The chiropractic sessions included long-axis traction maneuvers. Over nineteen years of treatment, Bronneke eventually alleged that Dr. Rutherford failed to disclose material risks and that his continuing treatment fell short of accepted professional standards in his field.
On appeal, the Nevada Supreme Court considered whether the informed consent doctrine applied to non-physician providers and whether the professional-standard disclosure test governed such claims. The Court reaffirmed that liability is measured by what a reasonable practitioner in the same specialty would disclose rather than a “reasonable patient” standard, and held that expert testimony must establish customary disclosure practices.
The decision in Bronneke clarified that Nevada’s informed consent framework applies uniformly to licensed healthcare providers—not just physicians—and that valid consent under this doctrine depends not only on patient authorization but on disclosure adequacy proven by expert testimony.
For practitioners, Bronneke reinforces the need to treat consent documentation and disclosure standards with the same rigor used in malpractice claims and alerts non-physician providers that the professional standard applies equally.
Evolving Standards in Nevada Malpractice Law
Recent rulings have consistently focused on NRS 48.035(1), admitting consent evidence only when directly relevant to the issues. Courts distinguish patient knowledge, relevant to assumption-of-risk defenses, from provider disclosure, which governs standard-of-care determinations. Practitioners must align evidence presentation with the precise theory of liability.
When consent adequacy is challenged, Nevada applies a subjective causation standard: plaintiffs must demonstrate that they would have personally declined treatment if properly informed. Meeting this burden requires expert testimony establishing customary disclosure practices, the materiality of undisclosed risks, and the effect of nondisclosure on the individual patient’s decision.
Strategic Implications for Legal Practice in Nevada
Nevada’s informed consent landscape requires early evaluation of evidentiary limits shaping case preparation and settlement strategy. Both plaintiff and defense counsel must adapt to rulings that restrict the admissibility of consent documentation when consent validity is uncontested.
Plaintiff Strategy Adaptations
For plaintiffs, the decision to challenge consent determines the entire evidentiary landscape. Contesting consent opens the door to assumption-of-risk defenses, while preserving consent validity bars such evidence and strengthens focus on breach and causation. Discovery should assess consent documentation early to identify disclosure deficiencies that may justify a challenge despite the added defense risks, and expert analysis should be coordinated from the outset to establish disclosure standards and causal links if consent validity becomes contested.
Defense Strategy Transformations
When consent is uncontested, defense counsel lose traditional reliance on consent forms and must pivot to expert testimony on surgical technique, complication rates, and alternative causation. Early case assessments should gauge whether plaintiffs will challenge consent to define available defensive approaches and expert needs.
Defense counsel should:
- Identify at the outset whether plaintiffs will contest consent validity to define expert strategy.
- Prepare experts to address surgical technique and alternative causation rather than consent documentation.
Settlement Negotiation Dynamics
Exclusion of consent evidence alters settlement leverage by removing a core defense tool. Defendants face greater exposure, while plaintiffs gain negotiating strength. However, sides must weigh expert-testimony burdens and timing pressures influencing settlement value.
Emerging Developments in Nevada Medical Malpractice Law
Nevada’s medical malpractice landscape continues to evolve as courts refine evidentiary standards governing consent-related issues. Recent rulings emphasize strict adherence to expert testimony requirements while narrowing admissibility to evidence that directly relates to contested negligence claims.
Key trends include:
- Heightened relevance scrutiny: Courts applying NRS 48.035(1) increasingly exclude consent evidence that lacks a direct connection to the alleged negligence.
- Expansion across specialties: Trial courts are extending these standards beyond surgical claims to other medical fields, signaling broader applicability.
- Strategic realignment: Defense teams are reassessing discovery priorities and expert selection in anticipation of a limited evidentiary scope.
Practitioners continue monitoring how Nevada courts interpret consent evidence across varying fact patterns to forecast litigation risks and settlement dynamics.
In Summary
Nevada’s informed consent jurisprudence balances statutory protection for providers with evidentiary standards, ensuring relevant evidence reaches juries. Recent developments narrow traditional defense options while clarifying how consent documentation interacts with professional negligence claims.
For practitioners, the priority is strategic decision-making around consent challenges and evidence presentation. Consent procedures remain vital for compliance and risk management, but cannot replace proper medical care. Understanding what consent evidence is admissible and under what circumstances is now central to an effective malpractice strategy.
The evolving framework demands early evaluation and disciplined planning for expert testimony. Firms that adapt to these standards while preserving sound trial practice will be best positioned for successful outcomes in Nevada medical malpractice litigation.







.webp)
.webp)