Medical records serve as foundational evidence in personal injury and medical malpractice litigation, with several record types providing critical legal information to prove liability, establish causation, and quantify damages.
These records must be retrieved and organized before legal analysis can begin. Understanding the structure and purpose of each medical record type helps legal teams identify what matters most, properly organize evidence, and reduce the time spent on repetitive document processing.
This article outlines 15 types of medical records most relevant to personal injury litigation, explaining what each contains and how they support legal arguments.
Why Understanding Medical Record Types Saves Time and Improves Case Outcomes
Case analysis depends upon access to complete medical records. As such, record retrieval is the primary procedural barrier to case preparation.
Requesting the right record types upfront prevents incomplete productions and costly re-requests. It also helps to:
- Prevent duplication.
- Accelerate discovery.
- Strengthen demand letters.
When legal professionals understand that emergency department records serve different evidentiary purposes than operative reports, they can review strategically rather than linearly through hundreds of pages.
For senior paralegals, mastering medical record structures offers both a time advantage and a professional differentiator. This expertise transforms document-heavy work into strategic analysis, allowing more time for case building and expert collaboration.
The impact extends beyond efficiency. Proper record classification ensures comprehensive discovery requests, prevents the omission of critical documentation, and supports expert testimony with a complete evidentiary foundation.
How Are Medical Records Classified?
Medical records generally fall into three operational dimensions that govern both legal access and strategic deployment in litigation.
1. Format and System Classification
Medical records are stored and accessed in various formats: paper files, Electronic Medical Records (EMRs), Electronic Health Records (EHRs), and hybrid systems.
- EMRs serve as organization-specific digital patient charts.
- EHRs consolidate patient data across multiple healthcare providers.
The distinction affects discovery scope and authentication procedures under the Federal Rules of Evidence (FRE).
2. Functional Content Categories
Functional records separate four primary content types: clinical documentation, diagnostic data, administrative records, and billing information.
- Clinical notes narrate treatment decisions and progress.
- Diagnostic reports capture objective test results.
- Administrative records demonstrate procedural compliance.
- Billing files quantify economic damages.
3. Legal Classification Framework
Under the Health Insurance Portability and Accountability Act’s (HIPAA) “designated record set” definition (45 CFR § 164.501), discoverable records include medical and billing documentation maintained by providers and health plans. Materials outside this scope—such as peer review files or psychotherapy notes—receive distinct legal protections.
Understanding these classifications ensures complete record requests and reliable documentation for expert review.
The 15 Types of Medical Records Every Legal Professional Should Know
1. Emergency Department Records
Definition: Document initial injury presentation, triage decisions, diagnostic workups, and immediate treatment responses.
Key Elements:
- Triage time stamps.
- Vital signs.
- Provider observations.
- Pain assessments.
- Documented delays in care.
Legal Significance: Establish causation timelines and injury severity baselines. Sequence accuracy and consistent provider observations strengthen evidentiary reliability.
2. Admission & Discharge Summaries
Definition: Define hospitalization scope, treatment objectives, and outcome evaluations.
Key Elements:
- Admitting versus discharge diagnoses.
- Length of stay justifications.
- Discharge planning decisions.
Legal Significance: Provide a comprehensive account of treatment scope and recovery trajectory, essential for quantifying damages. Discrepancies between admitting and discharge diagnoses may indicate diagnostic errors or treatment complications.
3. History & Physical (H&P) Reports
Definition: Establish a patient’s baseline health status, prior conditions, and initial clinical assessment.
Key Elements:
- Documented preexisting conditions.
- Physical examination findings.
- Patient complaint descriptions.
Legal Significance: Support causation analysis by distinguishing new injuries from preexisting conditions. Thorough identification of prior conditions strengthens damage calculations and settlement accuracy.
4. Progress & Encounter Notes
Definition: Record the progression of care decisions, treatment responses, and patient-reported outcomes over time.
Key Elements:
- Treatment effectiveness.
- Symptom progression.
- Patient complaints.
- Provider decision-making rationales.
Legal Significance: Document pain, suffering, and ongoing impairment. Identifying improvement or deterioration trends supports future care projections and damage quantification.
5. Operative & Procedure Reports
Definition: Detail surgical or procedural interventions, techniques applied, intraoperative findings, and complications.
Key Elements:
- Applied procedural techniques.
- Intraoperative findings.
- Complications.
- Deviations from standard procedures.
Legal Significance: Serve as primary evidence for standard of care analysis and procedural necessity evaluation. Highlighting complications or deviations supports causation arguments and expert witness preparation.
6. Consultation Reports
Definition: Record specialist evaluations, second opinions, and interdisciplinary care recommendations
Key Elements:
- Specialist recommendations.
- Provider disagreements.
- Follow-up compliance documentation.
Legal Significance: Demonstrate adherence to or deviation from the standard of care. Linking consultant recommendations to subsequent provider actions helps identify care coordination gaps or failures.
7. Laboratory & Pathology Reports
Definition: Contain diagnostic test results and pathology findings supported by clinical interpretation.
Key Elements:
- Abnormal results.
- Reference ranges.
- Critical values.
- Pathologist interpretations and staging information.
Legal Significance: Provide objective medical data supporting diagnoses and treatment decisions. Correlating abnormal findings with treatment responses reinforces causation and medical credibility.
8. Radiology & Imaging Records
Definition: Include imaging studies, radiologist reports, and comparative imaging results over time.
Key Elements:
- Radiologist interpretations.
- Comparison studies.
- Technical adequacy.
- Imaging protocol compliance.
Legal Significance: Offer visual, objective evidence of injury existence, extent, and progression. Linking images with interpretation notes strengthens causation and supports injury evaluation accuracy.
9. Medication & Prescription Records
Definition: Track prescribed medications, dosage adjustments, and documented compliance or adverse reactions.
Key Elements:
- Prescription timing.
- Dosage changes.
- Documented drug interactions.
- Compliance verification.
Legal Significance: Demonstrate treatment adherence and identify potential medication errors or contraindications. Discrepancies between prescribed and administered drugs may reveal care quality issues or affect recovery outcomes.
10. Therapy & Rehabilitation Notes
Definition: Document rehabilitation progress, functional assessments, and long-term treatment plans.
Key Elements:
- Functional improvement measurements.
- Progress measurements.
- Treatment modifications.
- Limitations or ongoing restrictions.
Legal Significance: Quantify recovery progress and project future care needs. Objective measures of improvement or ongoing impairment support both economic and noneconomic damage evaluations.
11. Nursing Notes & Vital Sign Charts
Definition: Capture continuous patient monitoring, medication administration, and real-time clinical observations.
Key Elements:
- Vital sign trends.
- Medication administration times.
- Patient responses.
- Care omissions or delays.
Legal Significance: Provide detailed chronological insight into daily care. Identifying timing gaps or omissions helps establish or refute allegations of negligent monitoring or delayed intervention.
12. Mental Health & Counseling Records
Definition: Include psychological assessments, psychiatric evaluations, and documentation of mental health impact from injury or trauma.
Key Elements:
- Psychological diagnoses.
- Treatment recommendations.
- Mental health impact assessments from injuries.
Legal Significance: Support claims involving emotional distress or psychological injury. Must be handled with heightened attention to privilege and consent requirements to maintain compliance with confidentiality laws.
13. Billing & Insurance Records
Definition: Provide documentation of treatment costs, billing codes, and insurance payment details.
Key Elements:
- Treatment coding accuracy.
- Billing timelines.
- Payment and denial records.
Legal Significance: Quantify economic damages and confirm the necessity of treatments rendered. Cross-referencing billed services with medical documentation ensures damage claims are complete and defensible.
14. Legal & Administrative Records
Definition: Include incident reports, informed consent documentation, and administrative compliance materials.
Key Elements:
- Signed consent forms.
- Incident report details and timing.
- Administrative policy compliance documentation.
Legal Significance: Establish adherence to administrative protocols and procedural safeguards. Comparing consent signatures, incident timing, and internal reports helps identify potential lapses that support negligence claims.
15. Electronic Systems (EMRs, EHRs, PHRs)
Definition: Describe digital systems for recording, managing, and sharing patient data across care providers.
Key Elements:
- Audit trail completeness.
- User identification and access logs.
- Modification timestamps.
- Data integrity verification.
Legal Significance: Offer comprehensive visibility into treatment records and care chronology. Complete audit trails and metadata authentication ensure data reliability and reveal post-incident alterations affecting evidentiary admissibility.
Further Compliance and Evidentiary Considerations
Under federal privacy regulations, only records within the designated HIPAA “record set” may be requested or produced in litigation. From an evidentiary standpoint, these boundaries determine what parties may disclose, authenticate, and introduce at trial.
- Protected and Privileged Materials
Certain records remain confidential despite inclusion in broader medical files. Psychotherapy notes, peer review documentation, and quality assurance materials are typically exempt from discovery, while substance abuse treatment records require specific authorization under 42 CFR Part 2.
- Record Retention and Preservation
Most states mandate medical record retention for seven to ten years, with extended periods for minors or active litigation cases. Healthcare providers must maintain originals or certified copies that preserve evidentiary integrity.
- Authentication and Chain of Custody
Under Federal Rules of Evidence 803(6), records require either custodian testimony or self-authentication. Electronic systems record metadata—user identifiers, timestamps, and audit trails—and legal teams verify it to confirm authenticity. Maintaining chain-of-custody documentation ensures reliability from creation through trial presentation.
Turning Record Literacy Into a Strategic Advantage
Mastering medical record types transforms case preparation from administrative work into strategic advocacy. When attorneys and paralegals understand how each record supports liability, causation, and damages, they build stronger, faster, and more defensible cases.
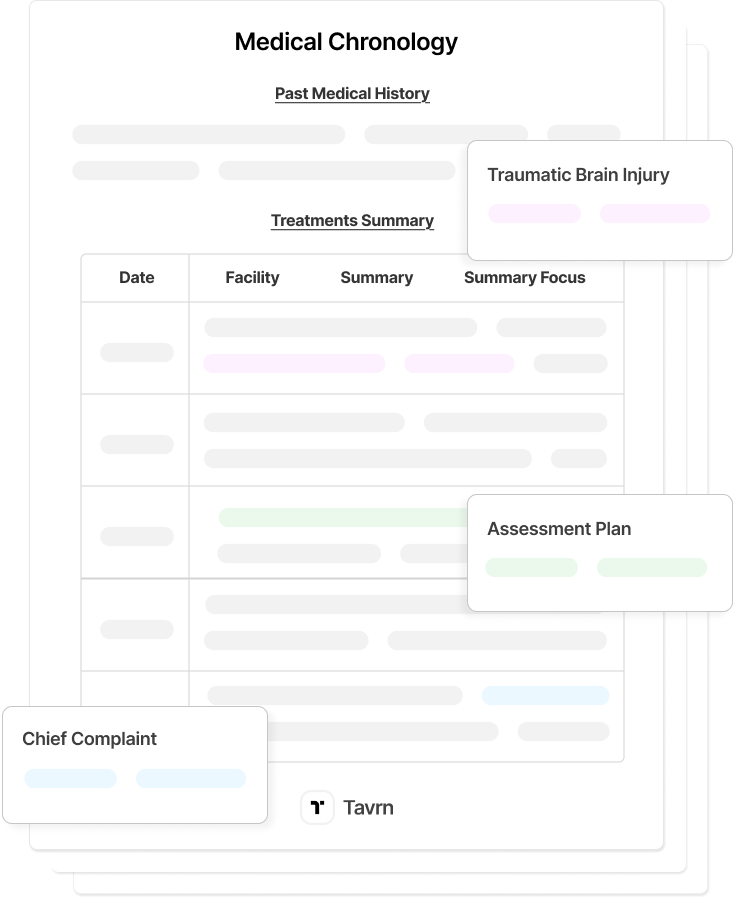
Tavrn streamlines medical record review with automated categorization, chronology generation, and source linking. Legal professionals receive clear, structured timelines with original data integrity and audit trails.
To accelerate your medical record review process, strengthen your case narratives, and elevate your firm’s litigation efficiency, try Tavrn.






.webp)
.webp)