Manual medical record retrieval creates recurring bottlenecks for paralegals managing dozens of active cases. The cycle repeats: submit authorizations, chase providers, receive partial records, and race discovery deadlines.
The question is not whether full records are needed, but whether to rely on voluntary retrieval or compel disclosure through subpoena.
This guide compares both and then details the compliant execution of a subpoena in accordance with HIPAA requirements.
What Is a Subpoena for Medical Records?
A subpoena for medical records is a court-mandated demand issued through subpoena duces tecum, requiring healthcare providers to produce specified documents. Unlike voluntary retrieval, subpoenas create legal obligations with enforcement mechanisms, including contempt-of-court sanctions for noncompliance.
According to HHS guidance, "a subpoena is not a court order", and this distinction affects HIPAA compliance obligations:
- Court orders signed by judges permit direct PHI disclosure.
- Attorney-issued subpoenas require either patient notification or qualified protective orders.
Attorneys commonly use subpoenas when voluntary cooperation fails, adversarial relationships exist with healthcare providers, litigation discovery deadlines approach, or comprehensive record production requires legal compulsion. They provide definitive authority to compel disclosure within specified timeframes, with timelines that vary by jurisdiction.
HIPAA Legal Framework for Medical Record Subpoenas
HIPAA Privacy Rule Section 164.512(e) establishes the regulatory framework for judicial and administrative proceedings. Healthcare providers may disclose PHI in response to subpoenas only when specific conditions are met: either reasonable patient notification efforts with opportunity to object, or qualified protective orders limiting PHI use and requiring record return after litigation concludes.
Patient notification requires written notice delivery to the individual's last known address, litigation disclosure informing patients of both legal proceedings and specific PHI requests, adequate response time allowing patients to object or seek judicial intervention, and documentation proving notice completion to healthcare providers.
Protective order alternatives must contain mandatory elements:
- Limitation clauses prohibiting parties from using PHI for purposes beyond the litigation.
- Return or destruction requirements mandating PHI disposal after case conclusion.
These orders grant healthcare providers HIPAA-compliant authority to disclose records without patient notification.
State Law Variations in Medical Record Subpoenas
State laws often impose additional protections beyond HIPAA, particularly for sensitive record categories. Common examples include:
- Mental Health Treatment Records: Often require court orders or explicit patient consent before disclosure.
- Substance Use Treatment Records: 42 CFR Part 2 governs these records and mandates judicial oversight
- HIV/AIDS Documentation: Subject to heightened confidentiality statutes and, in some jurisdictions, in-camera judicial review.
These safeguards vary significantly by jurisdiction, underscoring the importance of confirming local procedural requirements before proceeding.
Retrieval vs Subpoena: Strategic Analysis
Both retrieval and subpoena methods achieve the same objective—complete access to medical records—but through entirely different mechanisms. Understanding their comparative force, speed, and compliance obligations allows legal professionals to decide when voluntary cooperation suffices and when judicial authority becomes essential.
1. Legal Force and Enforceability
Retrieval depends entirely on voluntary provider cooperation, with no enforcement mechanisms when providers refuse or delay responses. Healthcare institutions can ignore authorization requests without legal consequence, creating unpredictable case preparation timelines.
Subpoenas carry court authority with contempt sanctions for noncompliance. Providers must respond within specified timeframes or seek judicial relief through motions to quash. This legal compulsion restores leverage when voluntary cooperation fails and provides a definitive resolution to record production disputes.
2. Speed and Timeline Control
Retrieval timelines vary dramatically based on provider responsiveness, ranging from rapid compliance to indefinite delays. Multiple follow-up communications consume paralegal time without guaranteed results, and providers often cite "processing backlogs" to justify extended delays.
Subpoenas establish definitive response deadlines that vary by jurisdiction and carry clear enforcement consequences. Court authority accelerates provider attention and creates predictable timelines essential for discovery management and settlement preparation schedules.
3. Risk and Compliance Burden
Retrieval carries minimal legal risk but creates operational risks through delayed case preparation and incomplete record production. HIPAA compliance remains straightforward with patient authorization, but success depends entirely on provider cooperation and internal processing capabilities.
Subpoenas require comprehensive HIPAA compliance, including patient notification procedures or protective order preparation. Procedural defects can result in contempt sanctions for attorneys, and improper PHI handling creates regulatory exposure for law firms managing sensitive medical information.
4. Scope and Control
Retrieval requests depend on the provider's interpretation of the authorization scope, often resulting in incomplete or selective record production. Providers may exclude relevant treatment notes, diagnostic imaging, or specialist consultations without clear justification or appeal mechanisms.
Subpoenas provide precise control over record scope through detailed document descriptions and specific time periods. Legal authority compels comprehensive production matching subpoena specifications, and objection procedures create clear resolution paths for scope disputes.
Choosing between record retrieval and subpoena is less about preference and more about leverage. Experienced paralegals recognize early when cooperation gives way to resistance and shift strategy before documentation delays threaten case preparation or discovery deadlines.
When to Subpoena Medical Records
Even under HIPAA’s Right of Access, voluntary retrieval depends on provider cooperation. The following scenarios signal that voluntary channels have reached their limits and a subpoena becomes imminent:
- Provider non-response after follow-ups. When healthcare providers fail to acknowledge authorization requests within 30 days or to provide an estimated completion date, voluntary cooperation has effectively failed, and legal compulsion becomes necessary.
- Incomplete or selective record production. Providers who return partial treatment histories, omit specialist consultations, or exclude diagnostic imaging without explanation typically continue selective disclosure patterns despite additional authorization requests.
- Imminent litigation or discovery deadlines. Approaching depositions, expert disclosures, or settlement conferences creates strict time pressures that retrieval cannot meet. Subpoena authority ensures comprehensive production within enforceable timelines.
- Adversarial or restrictive provider relationships. Some healthcare entities refuse disclosure even with valid authorizations, claim records are unavailable, or enforce internal policies that obstruct release. Legal compulsion restores balance and enforces compliance.
- Noncooperative third-party custodians. Large hospital systems, specialty practices with limited legal staff, or multi-network providers often require complex approvals that exceed case preparation schedules. Subpoenas streamline access through enforceable deadlines.
Once retrieval failures reach this stage, enforcement procedures become the next critical step in ensuring timely, complete production.
How to Execute a Subpoena for Medical Records
Once the decision to compel production has been made, the subpoena process defines how medical records enter the litigation record under enforceable authority. The following overview outlines the structural, compliance, and evidentiary standards governing the issuance and fulfillment of subpoenas.
Subpoena Validation and Assessment
Rule 45 of the Federal Rules of Civil Procedure establishes the procedural boundaries for subpoenas. Each document must include identifying case information, specific record descriptions, compliance deadlines, and proper signatures from the issuing attorney or court clerk. Federal place-of-compliance rules generally limit document production to within 100 miles of the record custodian’s location, though many parties arrange electronic delivery consistent with the rule’s intent.
The distinction between court orders and attorney-issued subpoenas determines how providers release protected health information under HIPAA. Court orders signed by judges authorize direct disclosure, while attorney subpoenas require either patient-notice procedures or qualified protective orders that meet the standards set forth in 45 CFR § 164.512(e).
Subpoena precision influences both compliance and response quality. Overly broad or vague document descriptions often lead to objections or partial productions. In contrast, well-defined treatment periods, provider names, and record categories reduce the likelihood of disputes and promote efficient fulfillment.
Handling Objections and Limiting Scope in Medical Record Subpoenas
Objections to subpoenas for medical records typically arise through motions to quash or limit disclosure. Healthcare providers may challenge the subpoena’s authority, invoke patient-privilege protections, or request judicial review to narrow its scope. Courts generally evaluate these challenges by examining subpoena validity, the sufficiency of HIPAA compliance, and the necessity of the requested medical information within the underlying proceeding.
Informal resolution often precedes formal motion practice. Counsel may negotiate scope adjustments, agree to redact particularly sensitive material, or stipulate to confidentiality measures that preserve privacy while maintaining access to relevant documentation. Such negotiated outcomes commonly shorten production timelines and reduce the administrative burden associated with extended litigation.
Protective orders function as the primary mechanism for balancing disclosure obligations with patient privacy. Courts frequently endorse limitations on PHI use, secure storage conditions, and controlled access provisions that satisfy both healthcare-provider concerns and evidentiary requirements within litigation.
Record Production and Quality Control Under a Subpoena
Record production standards emphasize accuracy and evidentiary integrity. Under Federal Rule of Evidence 902(11)–(12), business records are authenticated through custodian certificates identifying record origin, maintenance regularity, and verification under 28 U.S.C. § 1746.
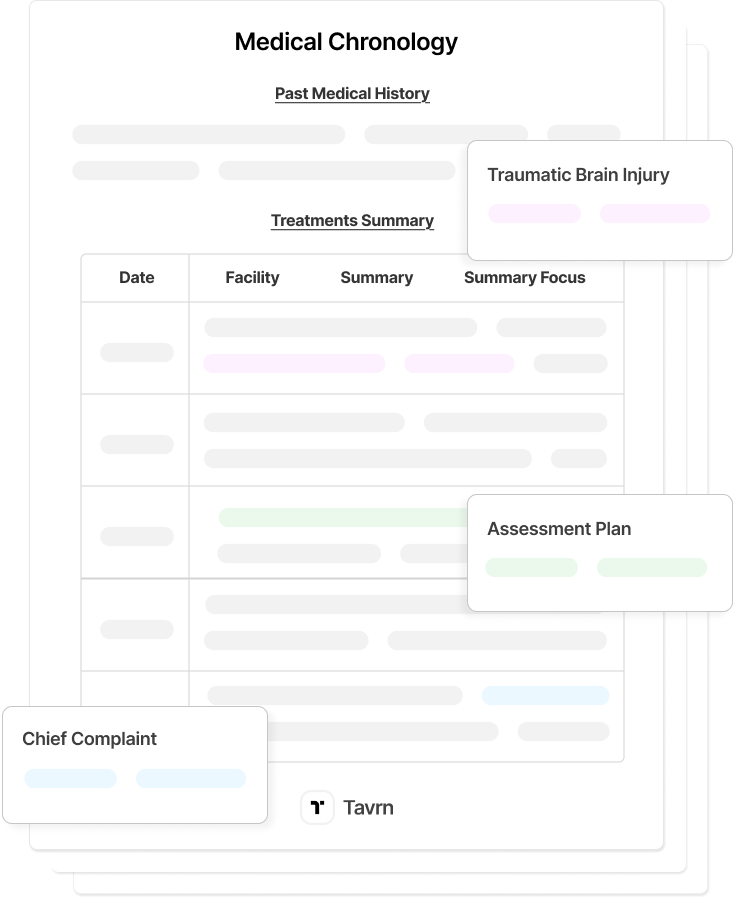
Organizational methods directly influence case preparation efficiency. Chronological sequencing, consistent file naming, Bates numbering, and cross-referencing systems support rapid review and settlement analysis. Legal AI platforms increasingly manage these functions, reducing manual processing and preserving paralegal attention for substantive case evaluation.
Quality control remains essential to completeness and defensibility. Received materials are measured against subpoena specifications, verified for authenticity through provider certification, and logged to document production accuracy for potential court review.
Subpoena execution ultimately balances procedural precision with privacy safeguards. When properly structured and monitored, the process produces defensible, authenticated records that strengthen the evidentiary foundation of personal injury and medical malpractice litigation.
Combining Medical Record Retrieval and Subpoenas
Parallel use of retrieval and subpoena mechanisms often improves efficiency in high-volume case preparation. Firms may pursue voluntary retrieval for cooperative providers while maintaining prepared subpoenas for those known to delay or resist disclosure. This dual-track process shortens overall timelines and preserves escalation options when voluntary cooperation stalls.
Targeted or partial subpoenas often address specific production gaps. Common use cases include:
- Missing treatment intervals where providers release incomplete chronological data.
- Unreturned specialist consultations that leave gaps in causation or damages analysis.
- Omitted diagnostic studies necessary for medical chronology or expert review.
Concentrating requests on these defined categories reduces redundancy and maintains procedural precision.
Protective orders and confidentiality stipulations remain effective tools for balancing disclosure obligations with privacy concerns. Courts routinely endorse reasonable limitations that satisfy provider compliance requirements while maintaining complete evidentiary access for litigation.
Ongoing evaluation of provider responsiveness, production completeness, and procedural timelines supports an adaptive approach. Systematic tracking reduces costs, minimizes duplication, and maintains compliance documentation across both retrieval and subpoena workflows.
Next Steps: Optimizing Your Record Workflow
Law firms can transform medical records management from a bottleneck into a competitive advantage through systematic workflows that handle both voluntary retrieval and subpoena requests while maintaining strict HIPAA compliance.
Effective record management requires systems that support both processes with equal precision, ensuring that access pathways remain compliant, documented, and repeatable.
The firms that master this dual capability transform medical record acquisition from reactive taskwork into structured, repeatable expertise.
Learn how Tavrn helps law firms manage medical record retrieval. Get a demo.







.webp)
.webp)