Every week, personal injury teams lose momentum while waiting for hospitals and clinics to release medical records. Each missing page causes delays in chronologies, demand letters, and settlement negotiations.
Medical records are the foundation of every personal injury claim. They establish causation, document treatment, and support the damages that determine settlement value. Because these records anchor every stage of litigation, timely retrieval is both a legal necessity and a strategic advantage.
This guide explains how to manage a personal injury medical records request. It covers why the records matter, who can request them, the steps for obtaining them under HIPAA, and how modern automation tools reduce waiting time to keep cases moving.
Why Do Medical Records Matter in Personal Injury Cases?
Medical records constitute the evidentiary foundation that proves causation, treatment necessity, and damages quantification in personal injury litigation. These documents serve as contemporaneous, objective evidence that establishes the three essential elements required for successful claims:
- Prove Causation: Emergency room reports and diagnostic imaging link the accident to specific injuries, refuting alternative-cause theories.
- Substantiate Treatment: Physician notes, surgical reports, and therapy summaries document the medical response, recovery timeline, and functional limitations.
- Quantify Damages: Billing statements and progress notes reflect both economic and non-economic losses, including pain, suffering, and emotional distress.
Well-organized medical records provide clear evidence that drives fair settlements and stronger leverage.
Who Can Request Medical Records in a Personal Injury Case?
HIPAA regulations define who has legal authority to obtain medical records. Patients hold direct access rights, while attorneys, paralegals, and other representatives must operate under valid authorization or legal process.
Patient Rights Under HIPAA
Under HIPAA’s Privacy Rule, patients may inspect and obtain copies of their own medical and billing records maintained by healthcare providers. Providers must respond within 30 days (with one 30-day extension if justified in writing) and may charge only reasonable, cost-based fees for copying or postage, but never search or retrieval fees.
Attorney and Paralegal Authority
Attorneys may request client records using a HIPAA authorization or through formal legal mechanisms such as subpoenas or discovery requests. A valid authorization must describe the information disclosed, identify both the disclosing and receiving parties, include an expiration date, and contain the patient’s signature with a right-to-revoke statement.
Paralegals can submit these requests under attorney supervision when acting on firm letterhead and following all federal authorization requirements. Proper oversight under ABA Model Rule 5.3 ensures compliance and professional accountability.
Special Circumstances: Deceased Clients, Guardianship, and Minors
HIPAA protections continue for 50 years after death. Executors or other legally recognized personal representatives have the same access rights as the deceased and may authorize disclosures on the estate’s behalf.
In guardianship or conservatorship cases, court-appointed representatives may obtain records relevant to their authority. For minors, access depends on state law—some jurisdictions grant parents full rights, while others restrict access to protect the minor’s privacy in certain healthcare contexts.
Defense Counsel Limitations
Defense attorneys and insurers have no automatic right to the plaintiff's medical records. They must obtain consent, issue properly noticed discovery requests, or secure a court order. HIPAA requires that individuals receive notice and an opportunity to object before any compelled disclosure occurs, protecting against overly broad record demands.
Step-by-Step: How Paralegals Request Medical Records for Personal Injury Cases
This six-step process provides paralegals with actionable protocols for efficiently managing multiple record requests.
1. Identify All Relevant Providers
Confirm every treating facility through client interviews, ambulance reports, pharmacy records, and billing statements.
- Contact each provider’s Health Information Management (HIM) department to verify submission requirements, accepted formats, and fee policies.
- Double-check provider details before sending authorizations to prevent rejections and missed facilities that slow production.
2. Prepare Required Authorizations
Draft a HIPAA-compliant authorization that lists the patient’s full identifiers, treatment date ranges, and purpose of disclosure. Include the recipient’s name, expiration date, and signature fields. Reviewing each authorization before submission ensures legal validity and avoids rejections that restart the retrieval timeline.
3. Submit the Request
Send requests using the provider’s preferred channel—secure portal, fax, mail, or encrypted email—and retain proof of submission. Keep a standardized log recording the method, date, and recipient. This documentation protects your team if disputes arise about whether or when a request was received.
4. Track and Follow Up
Monitor deadlines carefully under HIPAA’s 30-day rule, with a single 30-day extension allowed if justified in writing. Contact providers proactively around day 25 to confirm processing status and request extension notices when applicable. Consistent follow-up demonstrates diligence and helps prevent costly discovery delays.
5. Review and Organize Records
After receipt, cross-check files against billing statements and treatment dates to identify omissions.
- File records chronologically by provider and service date.
- Maintain an indexed summary listing provider, record type, and key findings to simplify causation analysis and demand-letter preparation.
Sometimes medical record requests are denied. In such cases, request a written explanation and pursue review rights under HIPAA. For incomplete or delayed records, send supplemental authorizations and log all communication attempts. Detailed tracking supports complaints or motions to compel if escalation becomes necessary.
Following these structured steps transforms record retrieval from a reactive task into a predictable, verifiable process that supports faster case preparation and stronger evidentiary control.
Legal and Privacy Requirements for Medical Record Requests
Medical record requests must balance efficiency with strict legal compliance under HIPAA and state privacy laws. Understanding these rules protects client confidentiality and keeps retrieval processes both lawful and efficient.
Core Compliance Principles:
- Limit scope: Under HIPAA’s minimum necessary standard (45 CFR §164.502 (b)), request only records relevant to the injury claim, specifying date ranges and providers directly related to treatment.
- Provider obligations: Covered entities must respond within 30 days (with one 30-day extension), charge only reasonable cost-based fees for labor and supplies, and provide written notice when access is denied.
- State law variations: Many states require faster response times (often 10–15 days), impose lower per-page fee caps, and add extra protection for sensitive records such as mental-health, substance-abuse, or HIV information.
- Fee limits: Federal law allows only cost-based fees for labor, supplies, postage, or summaries; several states further restrict these amounts or require reduced electronic-copy rates.
- Professional ethics: Attorneys must supervise staff to ensure compliance and maintain client confidentiality under ABA Model Rules.
Maintaining privacy compliance is not just regulatory; it reflects professional diligence. By narrowing requests, verifying provider billing, and supervising retrieval workflows, legal teams uphold both ethical standards and operational efficiency, minimizing risk while protecting client trust.
How AI-Powered Legal Tools Speed Up Personal Injury Medical Record Requests
Personal injury record retrieval is one of the most time-consuming phases of case preparation. AI-powered legal tools reduce delays by identifying missing information, accelerating provider communication, organizing incoming records, and strengthening causation analysis. These efficiencies help paralegals maintain case momentum and give attorneys earlier access to complete medical documentation.
1. Completing Provider Lists With Fewer Gaps
Missing providers create major delays and weaken causation. AI tools help uncover overlooked specialists, referrals, and one-off clinical visits that clients may forget to mention.
How AI Helps:
- AI reviews ER summaries, prescriptions, and treatment references to flag potential unreported providers.
- Systems like Tavrn automatically surface additional provider leads based on cross-referenced medical data.
- Paralegals can confirm the full list before requests go out, reducing follow-up rounds.
2. Reducing Provider Delays and Nonresponsiveness
Many facilities take longer than HIPAA allows. AI-assisted tracking reduces uncertainty by monitoring deadlines and escalating delays earlier.
How AI Helps:
- Automated workflows track all active requests and alert teams when response windows approach.
- Tavrn sends structured follow-ups and documents outreach for compliance and attorney review.
- Facilities that require escalation can be identified sooner, keeping case prep on schedule.
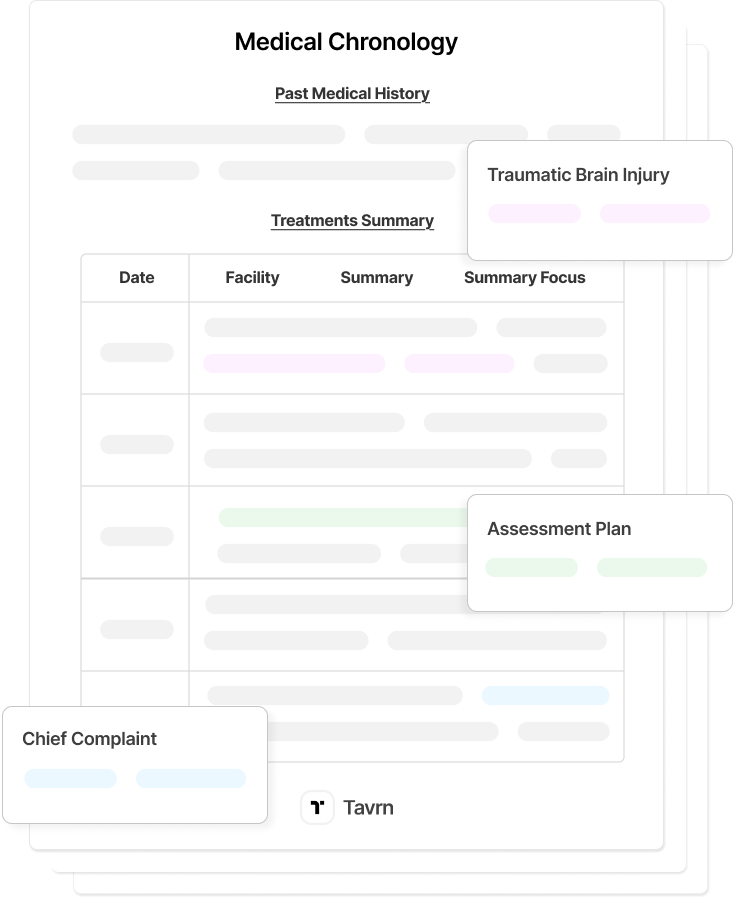
3. Organizing Incoming Medical Records Automatically
Disorganized, fragmented records slow down chronology creation and legal review. AI-driven organization saves hours of manual sorting.
How AI Helps:
- AI categorizes documents by provider, date, and record type on arrival.
- Tavrn organizes and hyperlinks records into structured, searchable formats tailored for legal review.
- Paralegals receive organized files instead of raw, unindexed PDFs.
4. Strengthening Causation Analysis Early
When records are scattered or unclear, defense counsel can challenge causation. AI helps reveal gaps or inconsistencies early enough for teams to address them.
How AI Helps:
- AI timelines identify unexplained gaps or conflicting notes.
- Tavrn maps treatment to incident-related injuries so attorneys can evaluate causation earlier.
- Paralegals can flag issues for expert review before negotiations begin.
Why This Matters for Personal Injury Teams
AI-powered record retrieval tools reduce repetitive admin work, accelerate document availability, and preserve evidentiary clarity. By pairing these workflows with a platform like Tavrn, legal teams shorten preparation time, maintain case momentum, and shift more hours toward analysis, valuation, and settlement strategy.
How to Optimize Medical Records Retrieval for Faster Personal Injury Case Preparation
A well-executed medical records request is the backbone of every successful personal injury case. Accurate, timely documentation strengthens causation, substantiates damages, and accelerates settlements by giving attorneys the evidence they need to negotiate confidently and build persuasive narratives.
AI-powered record retrieval systems, such as Tavrn’s, now manage the repetitive tracking, organization, and verification tasks that once consumed paralegal time. These platforms preserve critical attorney oversight while improving accuracy, transparency, and client responsiveness across every stage of case preparation.





.webp)
.webp)