Expert paralegals spend hours dissecting medical files, often uncovering the same documentation gaps that weaken liability arguments and delay case preparation. These recurring issues appear across nearly every malpractice file, regardless of firm size or specialty.
In medical malpractice litigation, missing information, inconsistent entries, and incomplete records directly affect how cases are valued and defended. Each error can distort causation, inflate damages disputes, or undermine expert testimony, creating costly inefficiencies during discovery.
This article examines the 15 most critical documentation failures found in malpractice litigation, outlining how each impacts case outcomes and how structured, systematic review methods help legal teams maintain accuracy, efficiency, and defensibility across every case.
How Medical Record Errors Affect Cases?
Medical record errors directly influence litigation outcomes. Even small documentation failures can weaken liability theories and delay settlements. According to Harvard’s Candello 2024 Benchmarking Report, documentation errors appear in about 20% of malpractice cases and more than double the odds of indemnity payments to plaintiffs.
For senior paralegals, these failures translate into practical risks such as:
- Weakened chronologies that disrupt causation timelines and reduce case defensibility.
- Higher expert costs when missing or inconsistent entries require supplemental review.
- Extended case preparation caused by fragmented, disorganized, or incomplete records.
The rise of electronic health records (EHRs) has amplified these challenges, introducing auto-fill mistakes, copy-paste inaccuracies, and system-generated inconsistencies that complicate discovery and increase liability exposure. Documentation quality now directly shapes both strategy and outcome: identification or consent errors can establish breach and causation, while metadata and audit trails in EHRs can reveal alteration patterns or institutional weaknesses.
Accurate, complete, and verifiable records reduce litigation uncertainty, support credible expert analysis, and give firms a stronger footing in negotiations and at trial. Consistent review standards and defensible documentation practices turn record management from a liability risk into a measurable litigation advantage.
15 Common Medical Record Errors
Recurring documentation failures are among the most common causes of weakened malpractice cases.
1. Incorrect Patient Identification
Misidentification—wrong name, date of birth, or record number—creates immediate evidentiary risk. Even a small mismatch can invalidate causation timelines or misattribute injuries.
To prevent identifier errors, review teams should:
- Verify identifiers consistently across all facilities and providers.
- Use at least two identifiers per Joint Commission protocol to confirm record accuracy.
- Employ AI-powered review systems to cross-check identifiers across full record sets, reducing mismatch risk while keeping documentation legally defensible.
2. Missing or Incomplete History/Allergy Documentation
Missing patient histories or allergy information directly impacts liability and expert review. Gaps can conceal known risks or prior conditions that change case interpretation.
To identify and close these gaps:
- Check intake forms and admission notes for absent allergy data or past diagnoses.
- Flag blank or duplicated sections that indicate incomplete charting.
- Use systematic record summaries to highlight missing clinical details early, reducing review time and strengthening defensibility.
3. Transcription or Charting Errors
Charting mistakes—wrong anatomy, uncorrected copy-forward text, or speech-recognition slips—can misstate events and compromise credibility.
To detect transcription inconsistencies:
- Compare dictated notes against operative reports for consistency.
- Watch for repeated phrasing that signals copy-paste documentation.
- Apply structured review tools that surface duplicate or contradictory entries quickly, allowing paralegals to focus on areas that need attorney validation.
4. Omitted or Delayed Test and Result Documentation
When orders and results don’t align, it suggests missed tests or unacknowledged abnormalities. Both create negligence exposure and weaken causation arguments.
To ensure test results are complete and accounted for:
- Match diagnostic orders to corresponding results chronologically.
- Flag unexplained gaps between testing dates and result entries.
- Use searchable timelines to trace diagnostic sequences and confirm whether results were reviewed or ignored.
5. Incorrect Medication Orders or Administration Entries
Medication discrepancies remain one of the most frequent causes of preventable harm. Documentation errors—wrong drug, dose, or missing confirmation—carry significant litigation risk.
To maintain medication accuracy across records:
- Cross-check medication orders, MARs, and nursing notes for mismatched details.
- Verify dosage changes or discontinuations appear consistently across providers.
- Use structured summaries to spot inconsistencies quickly and coordinate expert review before discovery deadlines.
6. Documentation, Authentication, and Timing Issues
Unsigned entries, missing timestamps, or back-dated notes undermine admissibility. They also suggest poor record-keeping or potential alteration.
To verify authenticity and timing:
- Confirm all entries have author names, dates, and times.
- Identify documentation made after adverse outcomes.
- Detect authentication gaps early to prevent spoliation disputes and protect case defensibility.
7. Inconsistent or Contradictory Documentation
When providers record conflicting findings—“stable” in one note, “critical” in another—it undermines reliability and inflates expert costs.
To reconcile contradictions effectively:
- Compare overlapping entries for the same encounter or condition.
- Highlight inconsistencies that affect causation or damage analysis.
- Use timeline views and linked source pages to isolate and resolve contradictions before trial preparation.
8. Wrong-Site or Side Documentation or Surgical Site Errors
Errors in surgical-site or side verification create automatic liability exposure and often qualify as “never events.”
To ensure procedural documentation accuracy:
- Verify site and side references match consent forms and operative notes.
- Ensure time-out checklists and signatures are complete.
- Maintain organized record sets for rapid confirmation of procedural accuracy and identification of Universal Protocol violations.
9. Missing or Inadequate Informed Consent Documentation
Absent or incomplete consent forms support claims of battery or negligent nondisclosure even when care itself was proper.
To confirm informed consent is complete:
- Confirm each procedure includes signed consent and documented risk discussion.
- Note missing pages or blank signature fields immediately.
- Use systematic retrieval to locate consent forms faster and flag any gaps for attorney review.
10. Record Management and Privacy Violations
Improper storage or unauthorized disclosure of protected health information (PHI) creates separate HIPAA liability in addition to malpractice exposure.
To verify compliance and prevent privacy breaches:
- Check that all authorization forms and disclosure logs are present.
- Identify misfiled or cross-referenced lab or imaging results.
- Maintain organized record delivery processes to reduce privacy risks and ensure PHI handling meets HIPAA and evidentiary standards.
11. Missing Follow-Up or Discharge Instructions
Discharge notes lacking next-step plans or patient-education details indicate continuity-of-care breaches.
To ensure proper follow-up documentation:
- Verify that follow-up appointments and patient instructions are documented.
- Flag generic or incomplete discharge summaries.
- Use chronology-based summaries to reveal these omissions and secure clarifying expert input.
12. Electronic Health Record (EHR) System-Related Errors
Digital records introduce new problems, such as duplicate entries, outdated copy-forward text, and auto-fill inconsistencies that distort timelines.
To detect and correct EHR-related issues:
- Review metadata and version histories (via audit trails and change logs) for edits after adverse events.
- Compare structured data against narrative notes for mismatched facts.
- Use AI-supported review tools to detect copy-paste cascades and fragmented documentation across systems.
13. Missing or Unclear Documentation of Patient Communications or Adverse Events
Unrecorded patient interactions or vague adverse-event notes weaken defense narratives and fuel discovery disputes.
To ensure all communications are properly documented:
- Confirm patient calls, complaints, and incident responses are logged with timestamps.
- Identify vague language like “discussed with patient” without context.
- Use structured indexing to capture and verify communications and event reports early.
14. Missing or Misfiled Imaging or Lab Attachments
Lost or misplaced diagnostics prevent full causation analysis and may suggest evidentiary mishandling.
To verify completeness of diagnostic documentation:
- Match all lab and imaging reports to orders and accession numbers.
- Note missing attachments or mismatched identifiers.
- Use organized retrieval systems to surface absent results quickly and keep defensible timelines.
15. Inadequate Documentation of Treatment Rationale
When clinical reasoning isn’t recorded, experts can’t assess care appropriateness, and plaintiff counsel can argue negligence by omission.
To ensure treatment rationale is complete:
- Check progress notes for differential diagnoses and decision explanations.
- Flag treatment plans lacking rationale or supporting data.
- Use detailed summaries to identify these omissions and strengthen expert support for defensible case narratives.
Each documentation failure weakens case defensibility and delays preparation. Detecting them early allows paralegals to maintain review consistency, strengthen evidence quality, and support more defensible case outcomes.
How Does AI Help Lawyers Mitigate Medical Record Errors?
Reducing documentation errors starts with creating structured review systems that balance speed and accuracy. Early use of AI-supported retrieval and chronology tools helps assemble complete, organized record sets, minimizing the inconsistencies that slow case preparation.
Key AI-driven practices that strengthen review accuracy include:
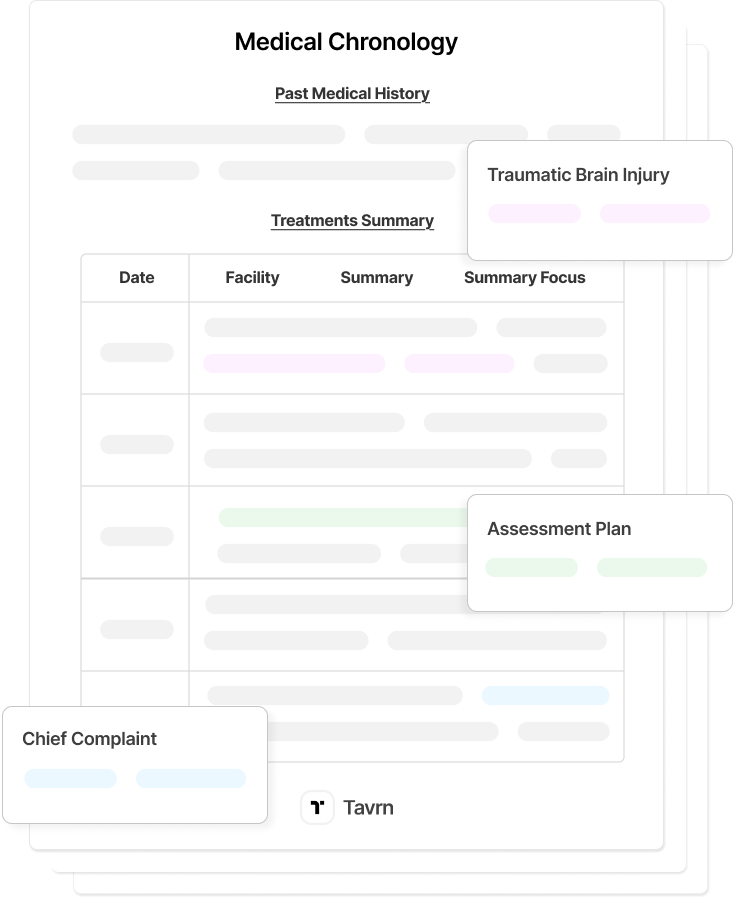
- AI-generated summaries and indexing: Legal AI platforms automatically categorize and summarize medical data, linking each event to its original source. This improves visibility across complex files and flags recurring documentation failures before they affect case analysis.
- Automated checklists and validation protocols: AI systems apply standardized checklists that detect missing pages, duplicated entries, or conflicting dates, maintaining consistency across teams and ensuring every record type receives equal scrutiny.
- Integrated expert consultation workflows: AI platforms connect medical findings directly to supporting evidence, enabling faster expert review and reducing time spent on manual cross-referencing.
Automation enhances these steps by streamlining organization and pattern detection, but professional oversight remains essential to verify accuracy and ensure that each conclusion drawn from the record is legally sound.
Transforming Medical Record Review Through Systematic Excellence
For senior paralegals managing complex litigation files, recognizing the 15 most common documentation errors is essential to improving accuracy and defensibility. Systematic review methods turn fragmented records into reliable evidence that supports stronger negotiation and trial strategies.
AI-powered tools such as Tavrn enhance these processes by organizing medical records, detecting documentation gaps, and structuring EHR data for faster, more consistent review. Automation accelerates analysis while attorney oversight ensures each output remains accurate and legally sound.






.webp)
.webp)