Medical record review determines case outcomes in personal injury litigation. The approach you select—or more accurately, the combination you deploy—shapes how effectively you establish causation, quantify damages, and build defensible settlement packages.
Most personal injury cases require multiple review approaches working together, not a single methodology. Early-stage case screening demands a different analysis than trial preparation. Compliance verification serves a distinct purpose from medical necessity analysis. Understanding each review type's primary function helps legal teams allocate resources strategically and avoid gaps in case preparation.
This guide examines seven review approaches that address different aspects of personal injury case preparation: initial screening, chronological documentation, evidentiary analysis, compliance verification, economic validation, pattern identification across cases, and technology-enabled automation. Each serves a specific purpose. Most comprehensive case strategies combine several.
Why is Legal Medical Record Review Important?
Precise medical record review determines how accurately a firm can quantify damages, connect injuries to specific incidents, document future care needs, and build a case.
Organized medical documentation supports credible damage calculations and counters defense arguments about causation or pre-existing conditions. Complete records enable attorneys to establish treatment timelines, verify medical necessity, and demonstrate injury progression with specific citations to source documents.
Review methodology affects case preparation timelines and documentation quality. Different case stages and complexity levels require different review approaches—often multiple types working in combination to address screening, chronology building, compliance verification, and economic analysis within a single matter.
Key Considerations for Medical Record Review
Comprehensive case preparation requires determining which review approaches to emphasize and how to sequence them effectively:
- Case stage: Early-stage matters prioritize screening reviews and case summaries for merit assessment. Advanced cases require detailed chronologies, compliance verification, and complete documentation for expert preparation and trial exhibits.
- Record complexity: Multiple providers, specialized conditions, or extended treatment timelines require chronological reviews and utilization analysis. Single-incident cases still need compliance verification and summary documentation, but with reduced scope.
- Intended use: Settlement negotiations depend on narrative summaries and medical necessity analysis. Trial preparation requires detailed chronologies with page-specific citations and complete compliance documentation.
- Internal capacity: Available paralegal hours, medical terminology expertise, and technology resources determine which review types a firm handles internally versus automating through AI-assisted tools.
- Compliance requirements: HIPAA authorizations, professional responsibility standards, and defensibility protocols apply across all review types and cannot be skipped regardless of case complexity.
7 Types of Medical Record Reviews
Each review type addresses a specific aspect of case preparation. Comprehensive cases typically combine multiple approaches—screening, chronological documentation, compliance verification, and economic analysis—rather than relying on a single methodology.
1. Case Overview / Summary Review
Summary reviews provide concise narratives that capture a case's medical storyline for fast evaluation.
When to Use: Early case screening, merit assessment, and intake prioritization, particularly in high-volume or mass tort practices.
Legal Value: Summaries highlight injuries, treatments, and recovery patterns, giving attorneys a clear understanding of case strength without exhaustive review.
Efficiency Angle: Condensed overviews allow firms to identify high-value cases early and allocate resources effectively during intake processes.
2. Medical Chronology Review
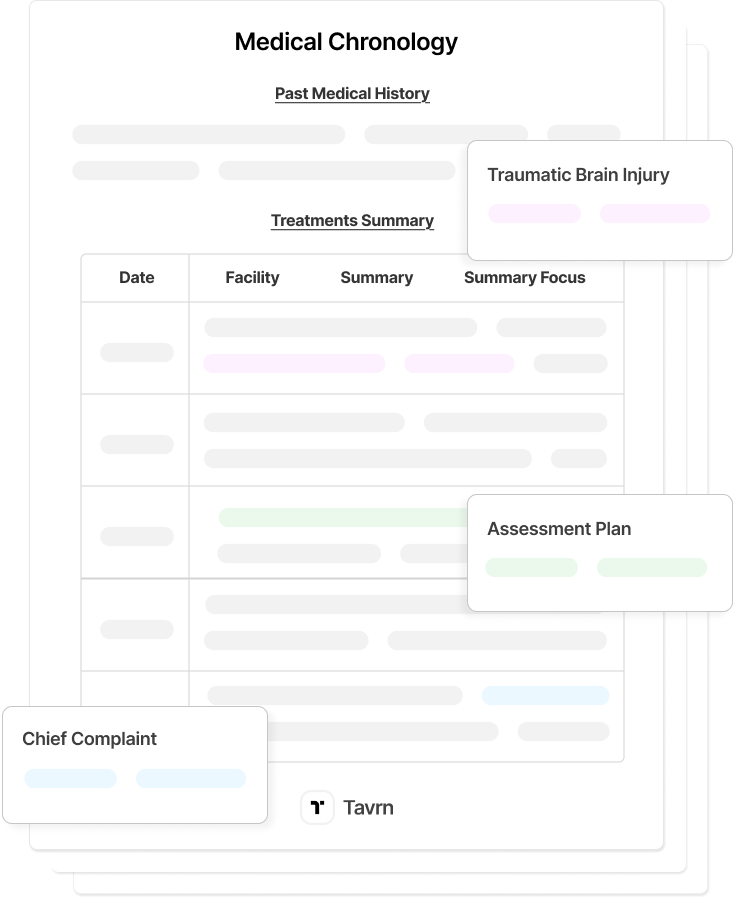
Chronologies organize patient histories into clear timelines that connect medical events to the underlying incident.
When to Use: All case stages, from initial evaluation to trial preparation, where timing and causation must be established.
Legal Value: Chronologies illustrate the progression of symptoms, treatment consistency, and causal links, helping attorneys validate damages and refute defense claims.
Efficiency Angle: A single, organized timeline replaces hundreds of pages of disjointed records, allowing attorneys and paralegals to locate key events quickly and focus on strategy.
Note: Many comprehensive case preparation workflows combine chronology review with summary documentation and compliance verification rather than treating them as separate processes.
3. Detailed Chart Review / Deep-Dive Review
Detailed reviews involve line-by-line analysis of medical records to build comprehensive chronologies and verify every data point.
When to Use: Complex or high-value cases requiring expert witness preparation, causation analysis, or precise courtroom references.
Legal Value: Detailed reviews ensure factual accuracy and defensibility, capturing every relevant note, dosage, and test result that supports expert testimony.
Efficiency Angle: Though time-intensive, detailed reviews prevent rework by eliminating gaps and providing complete, citation-ready medical evidence.
4. Compliance / Audit-Oriented Review
Compliance reviews verify that records are complete, properly authorized, and legally admissible.
When to Use: Required for all cases before discovery or trial to confirm HIPAA compliance, authentication, and redaction accuracy.
Legal Value: Prevents sanctions, inadmissibility challenges, and missing-document issues that can delay proceedings or damage credibility.
Efficiency Angle: Early verification ensures every record meets procedural and privacy requirements before substantive legal review begins, avoiding costly delays.
5. Utilization / Medical Necessity Review
Utilization reviews compare provided treatment to accepted standards of care, identifying excessive or missing services.
When to Use: Both plaintiff and defense cases to confirm the reasonableness of medical expenses and treatment necessity for damages calculations.
Legal Value: Supports damages calculations by distinguishing necessary care from unrelated or inflated billing, strengthening settlement positions.
Efficiency Angle: Focused analysis of billing and treatment data reduces disputes and clarifies the true scope of compensable medical costs.
6. Research / Cohort Review (Legal Research Context)
Research or cohort reviews analyze multiple case files to identify patterns across plaintiffs or populations.
When to Use: Mass tort or MDL litigation for identifying representative cases, trends, and general causation factors.
Legal Value: Consolidates data across claims to support bellwether selection and classwide arguments, ensuring consistency in evidence presentation.
Efficiency Angle: Standardized extraction methods streamline analysis across hundreds of records, reducing redundancy and ensuring uniform data quality.
7. AI-Augmented / Technology-Enabled Review
AI-assisted tools automate organization, extraction, and chronology generation while maintaining human oversight.
When to Use: Applies across all review types (#1-6) to automate document organization, data extraction, and chronology generation while maintaining professional oversight and legal defensibility.
Legal Value: Combines speed with defensibility by pairing automated data processing with attorney validation and contextual interpretation. End-to-end workflows from client intake through demand letter drafting maintain structured medical record data within unified platforms.
Efficiency Angle: Automation reduces time spent on document sorting and data extraction, allowing legal professionals to focus on case strategy and legal analysis rather than administrative processing.
Common Medical Record Review Errors
Even experienced legal teams encounter recurring mistakes during medical record review. Most errors stem from manual processes, fragmented data, and inconsistent provider documentation.
- Missing or incomplete records: One of the most frequent issues is relying on partial document sets. Missing charts, imaging results, or specialist notes can distort causation and damage calculations.
- Inconsistent timelines: Disorganized or misfiled entries make it difficult to connect treatment sequences, leading to errors in liability assessment or expert review.
- Ambiguous or misread documentation: Handwritten notes, unclear abbreviations, or duplicated pages often create confusion about patient progress and clinical findings.
- Unverified source material: Relying on summaries or scanned excerpts without confirming authenticity can undermine evidentiary integrity.
- Copied data without context: Extracting medical facts without linking them to corresponding records weakens the chronology and can compromise legal defensibility.
Each of these mistakes increases review time and elevates litigation risk. AI-assisted review tools can flag missing pages, standardize terminology, and detect inconsistencies across records, but professional verification remains essential for defensible outcomes.
How AI-Powered Medical Record Reviews Streamline Case Preparation
AI has transformed how legal teams handle medical record review, turning what was once a time-intensive, manual process into a structured and defensible foundation for case preparation. When combined with professional oversight, automation improves speed and accuracy across every review type.
AI systems now retrieve medical data, identify diagnoses, and organize treatment events into clear chronological timelines. What once required days of manual sorting can now be completed in hours, with hyperlinks connecting every data point to its original record for verification.
These capabilities enhance each core review type:
- Chronological reviews become automatically generated event maps that trace injuries, treatments, and outcomes across multiple facilities.
- Summary reviews are built from structured data, producing concise, fact-based narratives ready for negotiation and demand drafting.
- Detailed reviews benefit from AI’s ability to detect missing pages, inconsistent entries, or unexplained gaps before discovery deadlines.
Automation does not replace professional judgment; it amplifies it. Attorneys and paralegals remain responsible for validating all AI-generated materials and ensuring that findings align with case strategy and ethical standards.
Quality assurance remains central. Built-in audit trails, human verification, and confidentiality safeguards ensure every AI-assisted review meets the same professional standards as manual work. The result is a faster, more reliable, and legally defensible review process that lets legal teams focus their expertise where it matters most: analysis, argument, and settlement strategy.
Streamlining Case Strategy with the Right Medical Record Review Type
Effective case preparation combines multiple review approaches—screening, chronological documentation, compliance verification, and economic analysis—to build defensible evidence packages. Understanding which review types to emphasize at different case stages helps law firms allocate resources strategically.
AI-powered legal tools such as Tavrn accelerate medical record workflows across all review types. Automated organization and data extraction reduce repetitive document processing, while attorney oversight ensures legal judgment remains central to case strategy.





.webp)
.webp)