Medical record retrieval delays stall case preparation, compress discovery timelines, and leave paralegals chasing paperwork instead of building chronologies. Even a single missing record can undermine valuation and slow negotiations.
Medical record retrieval turnaround time measures the full period from submitting a request to receiving complete, authenticated records ready for legal review. Because these records anchor causation, damages, and settlement strategy, retrieval speed directly shapes case momentum.
This guide explains typical retrieval timelines, why delays occur, and practical strategies legal teams can use to set realistic expectations and improve turnaround time across personal injury and medical malpractice cases.
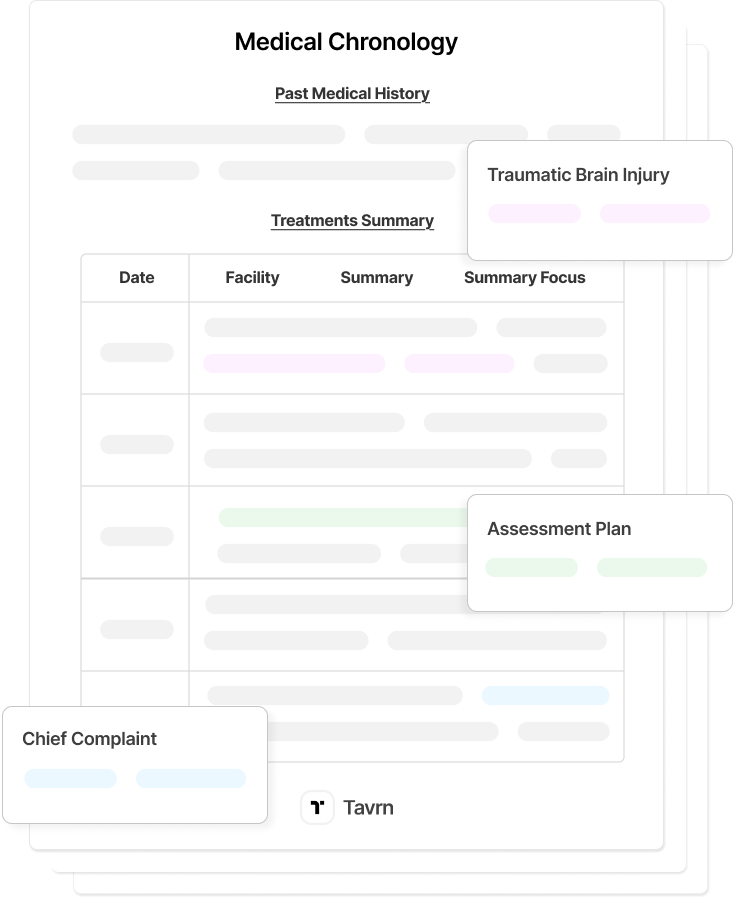
What Is Medical Record Retrieval Turnaround Time?
Medical record retrieval turnaround time measures the entire timeline from the initial request submission through the final delivery of organized, authenticated medical records ready for case preparation.
This process encompasses multiple stages:
- Authorization preparation and verification.
- Provider processing and internal coordination.
- Record compilation and organization.
- Final delivery with proper authentication.
In personal injury and medical malpractice workflows, complete medical records serve as prerequisites for:
Federal HIPAA regulations establish 30 calendar days as the maximum response time for properly authorized requests, with a single 30-day extension permitted. Yet this regulatory ceiling differs significantly from operational performance, particularly for complex cases that require multi-provider coordination or involve archived records systems.
Medical Record Retrieval Benchmarks
Most personal injury and medical malpractice requests fall in the 10 to 15-day range, with complex or multi-provider matters extending into 15 to 30+ days. Survey data is directionally practical but not definitive, and real-world timelines vary widely across providers and record systems. These ranges reflect practical experience across plaintiff firms, hospitals, and retrieval vendors, rather than rigid industry standards.
Industry Benchmark Numbers
The strongest available benchmark, U.S. Legal Support’s 2024 Litigation Support Trends Survey, reports an average turnaround of 10–15 days for standard cases using specialized retrieval services.
Complex, multi-provider, or specialty-driven matters routinely extend to 15–30+ days, especially when hospitals or paper-based archives are involved.
Variation by Context
Operational, technical, and legal factors shape turnaround time:
- Provider Infrastructure: Hospitals often require 15–30+ days; outpatient clinics typically complete within 10–15 days.
- Record Format: EHR systems average under two weeks; paper or archived files may approach HIPAA’s 30-day limit.
- Case Complexity: Single-provider requests complete fastest; multi-specialty or high-volume cases extend beyond typical ranges.
- Legal Request Scrutiny: Legal-use requests may undergo authentication, certification, and internal review, adding additional processing layers.
Plan for 10–15 days in straightforward, single-provider matters and 15–30+ days for multi-provider or specialized cases. Paper-based systems, archived files, or multi-jurisdictional records may require 45–60 days. Escalation is appropriate when providers exceed their stated timelines or approach the HIPAA 30-day limit without communication.
What Factors Affect Retrieval Turnaround Times?
Medical record delays usually fall into five categories: authorization errors, provider-side administrative bottlenecks, heightened scrutiny for legal requests, and multi-provider case complexity.
1. Authorization & Compliance Issues
Incomplete authorizations trigger immediate rejections and full resubmission cycles.
- Common issues include missing signatures, incorrect date ranges, and unclear or overly broad record scopes.
- Defective forms typically add 7–14 days to timelines.
- Even minor errors require complete reprocessing by providers.
- These are the most avoidable firm-side delays.
2. Provider Administrative Constraints
Provider-side bottlenecks slow processing even when requests are accurate and complete.
- Understaffed HIM/ROI teams face heavy volume and limited capacity.
- Fragmented entry points and non-centralized routing delay verification.
- Paper archives and outdated systems extend retrieval beyond standard timelines.
- These are external constraints that firms cannot directly control.
3. Legal Request Complications
Legal-use requests face stricter verification than routine patient requests.
- Providers add authentication layers to avoid HIPAA exposure.
- Records often require certification, pagination, and custodian affidavits.
- An internal legal or compliance review can add additional days.
- These are delays triggered by elevated scrutiny specific to litigation.
4. Multi-Provider Coordination Challenges
Cases involving multiple specialists or facilities extend timelines due to sequential processing.
- Each custodian requires separate authorizations and submission formats.
- Providers follow different procedural rules and turnaround expectations.
- Newly identified providers from initial records create additional request cycles.
- These delays grow with case complexity and provider count.
5. EHR Documentation & Finalization Gaps
Electronic records are not always fully documented or finalized at the time of request.
- Clinical notes may remain incomplete, unsigned, or pending revision.
- EHR workflows prioritize billing and treatment over legal retrieval.
- Delinquent documentation slows production regardless of authorization quality.
- These delays arise from provider-side documentation practices.
How Do Retrieval Delays Impact Litigation Timelines?
Medical record delays disrupt several core litigation milestones that depend on complete and accurate documentation. Mediation and early settlement planning often cannot proceed without updated treatment notes, imaging reports, or specialist evaluations, and key assessments of liability or damages remain incomplete until those records arrive.
Delays also affect expert involvement and discovery preparation. Experts cannot review partial files, and discovery responses may need extensions when documentation is still pending. These timing issues become more pronounced in high-volume practices where multiple cases enter preparation stages at once.
- Settlement and mediation dates may shift when records arrive behind schedule.
- Expert reports, rebuttals, and disclosures depend on complete documentation.
- Discovery responses are harder to finalize without updated or missing records.
Reliable access to full medical files helps firms maintain consistent progress across these milestones and reduces the risk of compressed preparation windows.
Best Practices to Improve Medical Record Retrieval Turnaround Time
Structured workflows, such as standardized authorizations, early submissions, tracked follow-ups, and provider-specific intelligence, create more predictable timelines.
Use Clear, Complete Authorization Templates
Accurate, HIPAA-compliant authorizations prevent the most avoidable delays. Forms must include all required elements under 45 CFR 164.508(c) and be correctly signed and dated.
- Clear identifiers, specific date ranges, and precise record descriptions.
- Separate forms for categories such as behavioral health, HIV/AIDS, and substance-use records.
Standardized templates and early verification help prevent rejections tied to jurisdiction-specific or facility-specific requirements.
Submit Requests Early and Expect Multi-Provider Involvement
Early submission at intake helps absorb real-world processing times. Initial records often reveal additional providers, which creates new authorization cycles.
- Additional custodians often appear only after reviewing first records.
- Each provider requires its own request and documentation.
Planning for multiple providers at the outset prevents avoidable delays created by sequential processing.
Use Digital Portals and Structured Follow-Up
Provider portals generally move faster than fax or mail, although managing multiple logins can add administrative load. Consolidating several authorizations for the same provider into a single submission reduces redundant steps.
A simple follow-up cadence, such as checks at day 7 and day 14 with escalation near day 30, keeps requests from stalling.
Combine Provider Relationship Intelligence and Specialist Retrieval Services
Tracking provider preferences, required forms, and submission methods improves first-pass accuracy. Retrieval partners can also coordinate high-volume, multi-provider cases more efficiently than internal staff when workloads spike.
- Useful for cases involving many facilities or out-of-state custodians.
- Reduces manual tracking for senior paralegals.
Combining internal knowledge with external support improves consistency, especially in complex or multi-specialty matters.
Monitor Turnaround KPIs and Track Requests in Real Time
Monitoring turnaround metrics helps firms identify delays before they affect case preparation. Key indicators include authorization preparation time, record receipt timelines, error rates, and cost per retrieval.
- Authorization prep under 3 days.
- Portal receipt within 5 days.
- Error rates below 1 percent and costs under 35 dollars per file.
Real-time tracking across all providers makes it easier to escalate requests when deadlines are at risk.
Integrate Retrieval Into Case Workflows
Coordinating retrieval with chronology development and early case assessment prevents gaps in preparation. Treating retrieval as part of the case lifecycle supports continuous progress rather than isolated administrative work.
This approach reflects NALA and CLOC guidance on connecting intake, record management, and downstream case development within a single workflow.
Establish a Provider Escalation Framework
Escalation protocols keep requests moving when providers fall behind and help document good-faith efforts to obtain records. A simple structure prevents long periods of inactivity and reduces avoidable delays.
- Confirm the request was received and accepted.
- Follow up using the provider’s preferred channel and document each contact.
If a facility remains unresponsive, firms can escalate to a supervisor or reference HIPAA’s 30-day requirement, with certified notices or subpoenas reserved for ongoing delays. A defined pathway gives case teams a predictable method for resolving stalled requests.
Why Law Firms Are Moving to AI-Powered Retrieval
Even with strong processes in place, manual retrieval hits a ceiling. Paralegals still spend hours preparing authorizations, tracking requests across portals, and following up with unresponsive providers. As caseloads grow, these tasks multiply—but staffing rarely keeps pace.
AI-powered retrieval removes these bottlenecks by automating the work that slows teams down:
- Authorization validation catches errors before submission, eliminating rejection cycles.
- Automated provider outreach sends requests and follow-ups without manual intervention.
- Real-time tracking surfaces stalled requests early, so nothing slips through the cracks.
- Multi-provider coordination runs in parallel rather than sequentially, compressing timelines on complex cases.
The result is faster access to complete records—without adding headcount or asking paralegals to do more with less. Firms using AI-powered retrieval consistently report shorter turnaround times and fewer administrative delays, freeing legal staff to focus on case strategy instead of chasing paperwork.






.webp)
.webp)