In Georgia, medical record delays prevent case preparation before legal analysis even begins. Senior paralegals managing several personal injury and medical malpractice cases face this bottleneck daily: weeks pass while waiting for providers to respond, creating cascading delays in chronology development, expert review, and settlement negotiations.
Legal professionals, especially paralegals overseeing large caseloads, rely on timely access to complete medical records to efficiently advance case preparation. Without these foundational documents, attorneys cannot properly evaluate case merit, establish damages, or proceed with substantive legal strategy.
This guide covers Georgia's statutory requirements, mandatory timelines, fee structures, and considerations for process efficiency.
Texas’s Legal Framework for Accessing Medical Records
Texas attorneys operate under a dual legal framework combining state and federal requirements that create stricter obligations than HIPAA alone.
- Texas Health & Safety Code Chapter 181 establishes state privacy and disclosure rules for entities handling protected health information, including organizations not otherwise subject to HIPAA (Chapter 181).
- Civil penalties under §181.201 may reach $5,000 per violation and up to $1.5 million annually for repeated non-compliance (§181.201).
- 22 Tex. Admin. Code § 76.3 requires fee notifications within 5 business days and payment within 10 business days, but imposes no production deadline after payment; it also sets maximum fees that differ by provider type (§76.3).
- HIPAA’s personal representative and legal-proceeding provisions—45 CFR 164.502(g) and 45 CFR 164.512(e)—remain fully applicable (HHS access guidance; HHS legal-proceeding FAQ).
- Attorneys are classified as “third parties” under §181.154, meaning subpoenas alone do not suffice without written authorization or a qualifying court order.
- In Scott v. Weems, the Texas Supreme Court held that disputes involving altered or fabricated medical records fall within Chapter 74’s definition of a health-care liability claim, triggering expert-report requirements (Scott v. Weems).
These authorities collectively define how Texas providers must handle requests, fee communications, and disclosures across both state and federal frameworks.
Georgia's Legal Framework for Accessing Medical Records
Georgia law provides clear statutory access rights through O.C.G.A. § 31-33-2, requiring providers to furnish medical records within 30 days of receiving a valid written request. This obligation applies to all records in a patient’s designated record set, including physician notes, diagnostic reports, imaging, and laboratory data. Records maintained electronically must be produced in electronic format upon request under § 31-33-8.
Key statutory exceptions include:
- Psychotherapy notes.
- Substance-abuse treatment records protected by 42 C.F.R. Part 2.
- Mental-health documentation under § 37-3-166.
- HIV-related information under § 24-12-21.
Beyond these narrow categories, providers may deny requests only for incomplete authorizations or unpaid fees. They cannot withhold records due to administrative burden, internal policy limitations, or concerns about litigation use.
Georgia courts treat timely production as a statutory obligation. In Woodard v. Gaines, the Court of Appeals noted that non-compliance may toll the medical malpractice statute of limitations when records are withheld. These timelines create predictable access standards and define the enforcement framework when providers fail to comply.
Who Can Request Medical Records in Georgia?
Georgia law and HIPAA limit medical record access to patients and clearly defined personal representatives. Under O.C.G.A. § 31-33-2, authorized requesters include individuals acting with valid legal authority, such as powers of attorney, guardianship orders, estate appointment documents, or properly executed patient authorizations.
Authorized requesters typically include:
- The patient.
- Healthcare agents under a power of attorney.
- Court-appointed guardians.
- Estate executors or administrators.
- Attorneys acting through a valid HIPAA authorization.
- Family members in the statutory order for deceased patients (executor → spouse → children → parents).
For deceased patients, Georgia’s statutory hierarchy governs who may request records—an important distinction in wrongful-death matters where multiple relatives may assert authority.
Identity verification applies to all requesters. Providers routinely require government-issued identification and supporting documents establishing representative authority (powers of attorney, guardianship papers, or estate letters).
HIPAA authorizations must contain all nine elements required under § 164.508, including a description of the information requested, authorized disclosers and recipients, purpose, expiration, signature, revocation language, and re-disclosure warnings. Authorizations missing any required element are invalid, and providers may refuse to process them.
Proper documentation streamlines the request process. Incomplete forms or missing authority documents lead to avoidable delays, while complete HIPAA-compliant submissions support timely production within Georgia’s 30-day statutory deadline.
How to Request Medical Records in Georgia: Step-by-Step Guide
Effective medical record requests require systematic preparation that satisfies both HIPAA and Georgia’s statutory rules. Standardized procedures help paralegal teams reduce delays and maintain predictable production timelines.
1. Identify Precise Record Categories
Record requests should specify treatment dates, provider locations, and the exact record types needed. Requests for “all records” without limitations increase costs and slow processing.
Georgia law requires providers to furnish records within 30 days of receiving a valid request, and fees must follow the statutory caps under § 31-33-3. Clear scoping helps avoid unnecessary volume and supports timely production.
2. Draft Complete HIPAA-Compliant Authorizations
HIPAA authorizations must include all nine required elements under § 164.508, including a description of information requested, authorized disclosers and recipients, purpose, expiration, and signature. Missing elements make authorizations invalid.
Personal representatives must also provide supporting legal documentation, such as powers of attorney or guardianship orders. Complete, compliant forms reduce provider rejections and avoid follow-up delays.
3. Required Documentation
Georgia requests must contain all required identifiers (patient name, DOB, contact details, provider information, dates, purpose, recipients, expiration, signature) plus HIPAA’s revocation and re-disclosure language. Providers frequently reject incomplete forms.
Personal-representative requests must also include legal authority documents—powers of attorney, guardianship orders, or estate letters—and photo ID for verification.
4. Submit Requests Using Provider-Preferred Methods
Providers process requests faster when submissions align with their preferred channels. Most Georgia systems accept fax, mail, secure email, or patient-portal uploads.
Always retain:
- Confirmation numbers.
- Fax receipts.
- Proof of mailing.
These records document compliance with Georgia’s 30-day deadline.
5. Delivery and Documentation Requirements
Teams should also document payment of any applicable statutory fees and maintain proof of delivery for each submission. These materials form part of the compliance record if production disputes arise or escalation becomes necessary.
6. Request Electronic Delivery
If records are maintained electronically, providers must supply them in electronic format under § 31-33-8. Electronic PDFs eliminate per-page copying fees and arrive faster.
Electronic files also streamline expert review and exhibit preparation. Requesting digital delivery at the outset prevents unnecessary paper production.
7. Maintain Updated Provider Contact Information
Provider submission procedures change frequently. Maintaining an updated internal directory reduces administrative rework.
Regular updates help teams anticipate processing timelines and avoid outdated fax numbers, email inboxes, or portal instructions.
8. Track the Mandatory 30-Day Response Deadline
Use calendaring tools to monitor the statutory deadline. Many teams set checkpoints on days 20, 25, and 30 to ensure consistent follow-ups.
Maintain a complete communication log with timestamps, receipts, and fee records. These materials support escalation through the Georgia Composite Medical Board if providers do not comply.
9. Develop HIPAA-Compliant Templates
Templates ensure that every request contains the required HIPAA elements and representative documentation. They also reduce drafting errors across high-volume matters.
For medical malpractice cases, templates should include forms compliant with § 9-11-9.2. Standardization improves accuracy and speeds preparation.
10. Conduct Quality Assurance on Receipt
When records arrive, verify that all requested date ranges and record types are present. Missing items should be noted immediately and followed up with supplemental requests.
Quality checks ensure accuracy before chronologies, summaries, or expert reviews begin. Early detection prevents downstream delays.
Georgia Medical Record Fees, Deadlines & Statutory Caps
Georgia caps medical record fees under § 31-33-3, with annual adjustments by the Department of Community Health. Providers must follow these limits or risk statutory violations.
Maximum fees effective July 1, 2025:
- $25.88 — search and retrieval.
- $9.70 — certification.
- Per-page copying:
- $0.75 (pages 1–20).
- $0.65 (pages 21–100).
- $0.50 (pages 101+).
Providers may charge actual postage but cannot add administrative or handling fees beyond the search-and-retrieval amount.
Electronic delivery is significantly cheaper because it eliminates per-page copying. A large paper set can exceed $300, while electronic delivery is limited to search, retrieval, and certification costs.
Georgia requires production within 30 days, with no state-level extensions. While HIPAA allows a single 30-day extension, Georgia’s statute controls and requires timely production or written justification citing the applicable legal basis.
Predictable fee structures and fixed timelines help legal teams budget accurately and assess record-retrieval strategies across different providers.
When Can Georgia Providers Delay or Deny a Medical Record Request?
Providers may delay or refuse medical record requests only in limited circumstances, such as invalid or incomplete authorizations, unpaid allowable fees, or requests involving protected categories (mental health, substance-abuse, or HIV/AIDS records). They may also deny disclosure when a clinician determines that release would endanger the patient or another person.
Any refusal must be issued within 30 days, include the specific legal basis, and provide appeal information. Failure to respond within the statutory deadline constitutes non-compliance. If disclosure to a patient is deemed harmful, providers may instead release records to a designated healthcare professional, though this exception does not apply to properly authorized attorney requests.
Georgia Composite Medical Board Escalation
When providers fail to comply, requesters may escalate through the Georgia Composite Medical Board.
Complaints should include:
- Copies of the original request and proof of delivery.
- Authorization documents.
- Correspondence logs showing follow-ups and deadlines.
- Evidence of statutory violations.
Maintaining organized timelines and documentation strengthens regulatory complaints and supports potential enforcement actions.
Improving Medical Record Retrieval Efficiency
Efficient medical record retrieval helps legal teams reduce delays created by manual requests, provider-specific procedures, and repeated follow-ups. Standardized authorizations, organized outreach, and clear deadline tracking give paralegals a more structured starting point and help firms obtain complete records before building chronologies or evaluating claims.
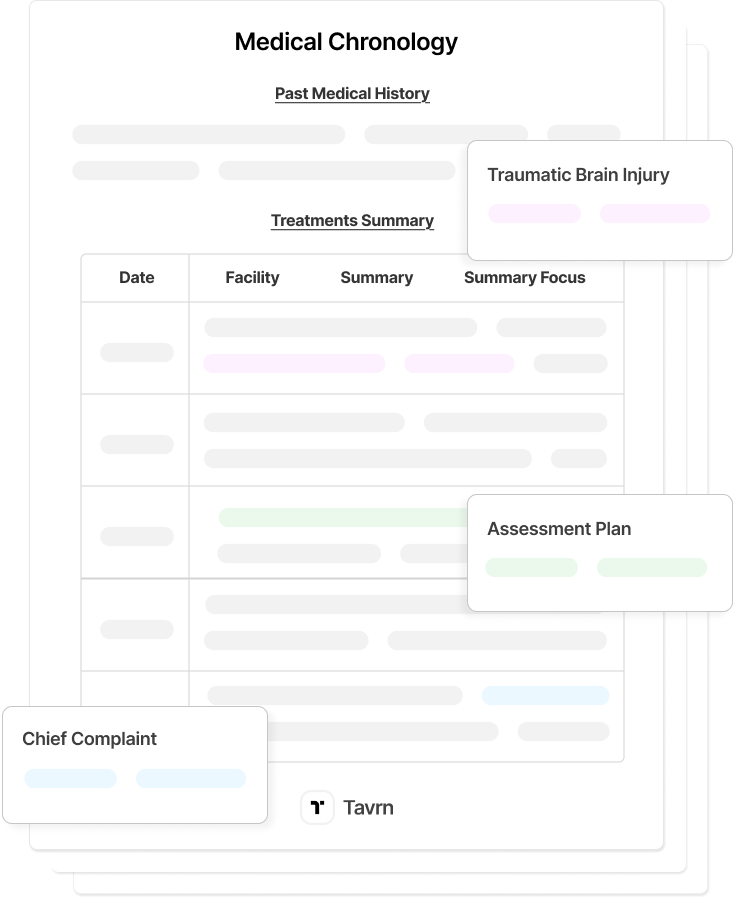
AI-powered retrieval tools, like Tavrn, reduce these delays by automating provider outreach, tracking responses, and consolidating released records into a single, review-ready set. Firms still verify completeness and maintain responsibility for HIPAA compliance, but automated retrieval shortens the time between initial request and substantive case work. Faster access to complete records supports earlier case evaluation, clearer documentation, and stronger downstream workflows.
Faster Medical Record Retrieval in Georgia
Georgia law and HIPAA establish defined access rights, but timely medical record production depends on clear requests, compliant authorizations, and consistent follow-up. Understanding deadlines, fee limits, and provider obligations allows legal teams to streamline retrieval and avoid unnecessary delays.
Tavrn supports this process by centralizing requests, ensuring compliant submissions, and reducing administrative back-and-forth across providers. With predictable turnaround times, legal teams can begin case evaluation sooner and maintain steady momentum throughout litigation.





.webp)
.webp)