In October 2006, a Hillsborough County, Florida jury returned a $216.8 million verdict after emergency department providers misdiagnosed Allan Navarro’s stroke as sinusitis. Although the case ultimately settled before appellate review, the verdict remains one of Florida’s largest medical malpractice awards involving emergency medicine.
The litigation arose before Florida's modern tort-reform framework and centered on diagnostic judgment, supervision practices, and institutional credentialing failures within a hospital emergency department.
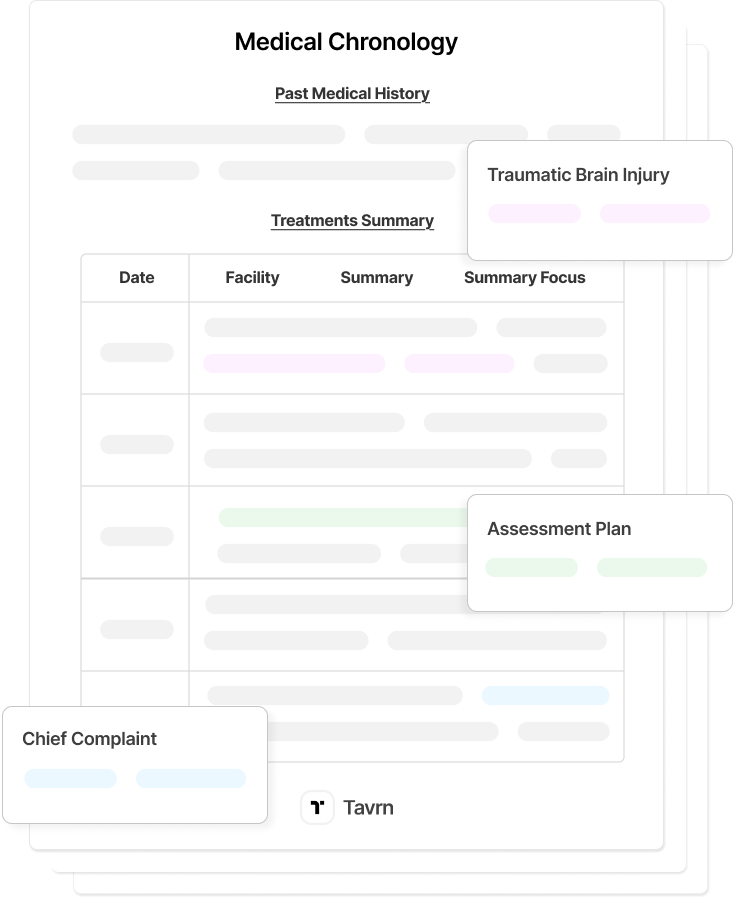
This analysis examines the factual record, procedural posture, damages allocation, and legal implications of the Navarro case within broader emergency medicine malpractice trends and historical damages benchmarks. For related context, see Tavrn's medical malpractice case analyses.
Stroke Misdiagnosis Allegations in the Allan Navarro Case
The core liability dispute in Navarro centers on whether emergency department providers recognized and appropriately responded to classic stroke symptoms during the patient’s initial presentation. The hospital encounter provides a detailed record for examining diagnostic decision-making, supervision protocols, and escalation failures in an emergency medicine setting.
Initial Emergency Presentation
Allan Navarro presented to University Community Hospital's Carrollwood campus emergency room in Tampa on August 9, 2000, at approximately 2:30 PM. Symptoms included sudden onset, severe headache with "pop" sensation, nausea, dizziness, and double vision—a constellation consistent with an acute cerebrovascular event.
Navarro disclosed multiple stroke risk factors: high blood pressure, high cholesterol, diabetes, and a family history of strokes.
Initial examination was conducted by Mark Herranz, a physician assistant whose licensure and credentialing status became a central issue at trial after evidence showed repeated failures to obtain Florida licensure and deficiencies in supervisory oversight. Dr. Michael Austin, the attending emergency physician, ordered CT scans interpreted as negative. Navarro received a diagnosis of sinusitis and was discharged with painkillers.
Plaintiffs framed this issue not as an isolated personnel failure, but as an institutional breakdown in credentialing and supervision protocols within the emergency department.
Catastrophic Neurological Decline
Following discharge, Navarro experienced confusion, vomiting, slurred speech, and inability to walk. He returned approximately 15.5 hours later. New imaging revealed a stroke, and an emergency brain surgery followed. Navarro remained in a coma for nearly three months.
Permanent disabilities included wheelchair confinement with loss of limb function except limited right arm movement, complete loss of bowel and bladder control, medical prohibition from eating solid food due to aspiration risk, and inability to lift his own son.
Procedural History of the Allan Navarro Malpractice Lawsuit
Procedurally, the Navarro litigation followed a conventional medical negligence trajectory through trial but ended in an atypical posture due to its post-verdict settlement. Understanding the named defendants, asserted theories, and settlement timing is necessary to place the verdict’s legal significance—and its limitations—into context.
The lawsuit, filed in Hillsborough County in 2002, named Dr. Michael P. Austin, Mark Herranz, and corporate defendants Franklin, Favata & Hulls, M.D.s, and Carrollwood Emergency Physicians.
Claims included medical negligence, failure to meet the standard of care, misdiagnosis, and wrongful injury. Insurance carriers offered only $300 total before the three-week trial commenced in October 2006. The case settled in March 2007 for an undisclosed amount before appellate proceedings.
Breakdown of the $216.8 Million Allan Navarro Verdict
The jury’s verdict in Navarro reflected an expansive damages assessment across economic, non-economic, and punitive categories. The allocation provides insight into how juries evaluate catastrophic neurological injury, lifetime care needs, and institutional conduct when supervision and credentialing failures are alleged.
Compensatory Damages: $116.7 Million
- Economic Damages (approximately $16.2 million): $15.6 million medical expenses; $615,000 lost wages and earning capacity.
- Non-Economic Damages (approximately $98.5 million): $9 million past pain and suffering, $37.5 million future pain and suffering, and $52.5 million wife's consortium claim.
Punitive Damages: $100.1 Million
Following approximately three hours of deliberation on compensatory damages, the jury deliberated approximately 30 minutes before returning the $100.1 million punitive award.
Liability Allocation:
- Dr. Michael Austin: 25%
- Mark Herranz: 25%
- Franklin, Favata & Hulls: 50%
Plaintiff counsel Steven Yerrid argued the jury should "send a message to doctors and insurance companies to never put profits over patient safety." The $300 settlement offer was highlighted as evidence of institutional disregard. The Navarro family pledged to donate the entire punitive award to charities supporting spinal cord and brain injury research.
Standard of Care and Causation Issues in the Allan Navarro Case
Liability findings in Navarro rested not only on diagnostic error but also on institutional compliance with licensure, supervision, and escalation standards. The plaintiff’s causation theory combined individual clinical failures with systemic oversight breakdowns, allowing the jury to assess both medical judgment and hospital governance.
Licensure Compliance as Central Issue
The licensure deficiencies associated with Mark Herranz became central to both liability and punitive damages findings. It supported direct evidence of institutional quality control failure, vicarious liability exposure for supervising physicians, a foundation for corporate negligence claims, and grounds for substantial punitive damages.
Diagnostic Protocol Failures
Expert testimony established specific standard-of-care deviations. Herranz failed to perform a complete neurological examination despite classic stroke symptoms. Defendants failed to order an MRI despite a negative CT scan when clinical suspicion remained high. The standard of care requires follow-up imaging when clinical presentation strongly suggests stroke despite negative initial CT results.
Legal and Policy Implications of the Allan Navarro Verdict
Although the Navarro verdict lacks precedential value, it remains relevant as a historical benchmark for damages exposure and emergency medicine liability. Its timing—before Florida’s modern tort-reform landscape—limits replication but informs contemporary valuation discussions and institutional risk assessment.
Pre-Tort Reform Damages Ceiling
The Navarro verdict was rendered before Florida imposed caps on certain malpractice awards, making its magnitude non-replicable under current law. Subsequent Florida medical malpractice verdicts have generally reflected lower damages exposure following the state’s evolving tort-reform landscape, limiting the likelihood of verdicts reaching Navarro's magnitude.
Because the case settled before appeals, it produced no published appellate opinion and has no citability as legal precedent in Florida courts. The verdict is useful only for historical damages benchmarking and settlement value discussions.
Emergency Medicine Diagnostic Standards
Recent Supreme Court decisions continue to refine standards relevant to emergency room diagnostic failure cases. The Arizona Supreme Court addressed causation standards in its 2025 decision in Henke v. Hospital Development of West Phoenix, Inc., while Idaho's 2025 decision in Hill v. Emergency Medicine of Idaho, P.A., examined evidentiary issues in stroke misdiagnosis. Emergency room diagnostic negligence doctrine continues to evolve.
Strategic Lessons from the Allan Navarro Malpractice Case
The litigation record continues to inform plaintiff, defense, and risk-management strategies in medical malpractice cases involving emergency care. The following takeaways reflect how credentialing, settlement posture, and documentation practices can materially influence trial outcomes.
For Plaintiff Counsel
- Systemic negligence framing elevates individual error to institutional failure.
- Pre-trial settlement conduct may serve as punitive damages evidence. The $300 offer proved critical.
- Licensure investigation may reveal credentialing failures supporting vicarious liability.
For Defense Counsel and Risk Management
- Unlicensed personnel credentialing failures expose institutions to substantial liability.
- Settlement authority and bad faith conduct can generate punitive damages exposure.
- Neurological assessment documentation failures prove fatal in stroke cases.
- Supervision and institutional oversight gaps generate corporate negligence liability.
Why the Allan Navarro Case Still Matters in Emergency Medicine Malpractice
The Allan Navarro verdict illustrates how diagnostic failure, supervision breakdowns, and credentialing deficiencies can combine to produce extraordinary jury outcomes in emergency medicine malpractice cases. Although the settlement foreclosed appellate review, the verdict remains a historical benchmark for catastrophic injury valuation.
Cases of this magnitude underscore the importance of comprehensive medical record development, credentialing analysis, and structured timelines when evaluating emergency department liability, even under modern tort-reform constraints.
Read more medical malpractice case analysis.






.webp)
.webp)