Texas medical record request laws are governed by state statutes and federal HIPAA requirements that define how patients and authorized representatives access medical documentation. These rules apply to physicians, hospitals, and other licensed providers across the state.
The framework includes authorization standards, fee-notification procedures, confidentiality provisions for sensitive record categories, and federal production timelines. Together, these authorities outline how records must be requested, processed, and released.
This guide details Texas’s access rules, request procedures, statutory fees, delivery formats, and oversight mechanisms. It also reflects operational considerations commonly encountered in routine record collection across personal injury and medical malpractice matters.
Texas’s Legal Framework for Accessing Medical Records
Texas attorneys operate under a dual legal framework combining state and federal requirements that create stricter obligations than HIPAA alone.
- Texas Health & Safety Code Chapter 181 establishes state privacy and disclosure rules for entities handling protected health information, including organizations not otherwise subject to HIPAA.
- Civil penalties under §181.201 may reach $5,000 per violation and up to $1.5 million annually for repeated non-compliance.
- 22 Tex. Admin. Code § 76.3 requires fee notifications within five business days and payment within 10 business days, but imposes no production deadline after payment; it also sets maximum fees that differ by provider type.
- HIPAA’s personal representative and legal-proceeding provisions—45 CFR 164.502(g) and 45 CFR 164.512(e)—remain fully applicable.
- Attorneys are classified as “third parties” under §181.154, meaning subpoenas alone do not suffice without written authorization or a qualifying court order.
In Scott v. Weems, the Texas Supreme Court held that disputes involving altered or fabricated medical records fall within Chapter 74’s definition of a health-care liability claim, triggering expert-report requirements.
These authorities collectively define how Texas providers must handle requests, fee communications, and disclosures across both state and federal frameworks.
Who Can Request Medical Records in Texas?
Texas law and HIPAA limit access to patients and clearly defined personal representatives. Under Texas Health & Safety Code § 161.0001, authorized requesters include parents or managing conservators of minors, court-appointed guardians, and agents acting under a valid medical power of attorney.
Authorized requesters typically include:
- The patient.
- Agents named in a durable power of attorney for health care.
- Court-appointed guardians for minors or incapacitated adults.
- Personal representatives of estates under the Texas Estates Code.
- Attorneys acting through a valid, HIPAA-compliant authorization.
For deceased patients, Texas Occupations Code § 159.005 limits access to court-appointed personal representatives, requiring supporting documents such as Letters Testamentary or Letters of Administration and government-issued identification.
HIPAA authorizations must contain all nine elements required under § 164.508, including a description of the information requested, authorized disclosers and recipients, purpose, expiration, signature, revocation language, and re-disclosure warnings. Authorizations missing any required element are invalid, and providers may refuse to process them.
For attorneys as third parties, subpoenas alone are insufficient; providers may release records only with a compliant authorization or a qualifying court order. Chapter 74 creates a narrow exception in medical malpractice matters, allowing certain family members—such as spouses or adult children—to authorize releases for health-care liability claims.
Proper authority documentation streamlines the request process, while incomplete or non-compliant authorizations may delay production under Texas and federal access rules.
How to Request Medical Records in Texas: Step-by-Step Process
Effective medical record requests require systematic preparation that satisfies both HIPAA and Texas’s statutory rules. Standardized procedures help paralegal teams reduce delays and maintain predictable production timelines.
1. dentify Precise Record Categories
Requests should specify treatment dates, provider locations, and the exact record types needed, such as progress notes, imaging, labs, and billing records. Broad requests for “all records” increase costs and slow production. Multi-facility systems require separate requests for each location.
2. Draft Complete HIPAA-Compliant Authorizations
Authorizations must include all nine elements required under 45 C.F.R. § 164.508. Texas also requires explicit written consent for sensitive categories, including mental health, substance-use treatment, HIV/AIDS information, and genetic data. Missing elements allow providers to reject the request.
3. Required Documentation
Texas requests must include all core identifiers—patient name, DOB, provider information, dates, purpose, recipients, expiration, and signature—plus HIPAA’s revocation and re-disclosure language. Personal representatives must attach legal authority documents such as powers of attorney, guardianship orders, or probate papers for deceased patients.
4. Submit Requests Using Provider-Preferred Methods
Texas providers commonly accept fax, mail, encrypted email, or patient-portal uploads. Retain confirmation receipts, proof of mailing, or portal acknowledgments to document when the request was received.
5. Delivery and Documentation Requirements
Maintain proof of payment for any fees and retain all correspondence. These materials support escalation if fee notices or production timelines are disputed.
6. Request Electronic Delivery
Electronic records reduce costs under Texas fee schedules and typically arrive faster. Digital files also streamline review and exhibit preparation.
7. Maintain Updated Provider Contact Information
Provider contact details and submission procedures change frequently. Updated directories help avoid outdated fax numbers, email inboxes, or portal instructions.
8. Track Fee Notification Deadlines
Under 22 Tex. Admin. Code § 76.3 requires providers to issue fee notices within 5 business days and to receive payment within 10 business days. Texas sets no production deadline after payment, so HIPAA’s 30-day timeline governs record release.
9. Develop HIPAA-Compliant Templates
Templates ensure each request includes all required HIPAA elements and Texas-specific sensitive-category authorizations, reducing errors and rejections.
10. Conduct Quality Assurance on Receipt
Verify patient identifiers, date ranges, and all requested record types. Follow up promptly if any items are missing.
Texas Medical Record Fees, Deadlines & Statutory Caps
Texas maintains three distinct fee structures depending on provider type—physicians regulated by the Texas Medical Board, hospitals under HHSC, and other covered entities under 22 TAC § 76.3—creating significant budget implications for personal injury and medical malpractice cases. Texas fee schedules vary by provider type, and maximum charges are set by state rule.
Physicians (Texas Medical Board)
- Paper copies: $25 for the first 20 pages, then $0.50 per page.
- Electronic format: $25 for ≤500 pages or $50 for >500 pages.
- Additional fees: up to $15 for affidavits; $8 per imaging study.
Hospitals (HHSC)
- Tiered paper pricing:
- Pages 1–10: $60.10 total
- Pages 11–60: $2.03/page
- Pages 61–400: $0.99/page
- Pages 401+: $0.54/page
- Electronic records: retrieval fees up to $108.89; written response fees up to $11.53.
Other Providers (22 TAC § 76.3)
- Digital-only requests: maximum $50 administrative fee.
- Paper copies: $25 for the first page, then $0.25/page.
- Imaging: $50 for the first page, then $1.00/page.
Electronic delivery typically reduces total costs under all three schedules.
Texas law requires providers to issue fee notices within five business days and receive payment within 10 business days, but does not specify any production deadline after payment. HIPAA’s 30-day release requirement (with one 30-day extension) therefore governs record production.
When Can Texas Providers Delay or Deny a Medical Record Request?
Texas providers may deny access only in narrow circumstances. Under Health & Safety Code § 611.0045, a licensed professional may withhold records if disclosure would harm the patient’s physical, mental, or emotional health. HIPAA likewise permits safety-based denials and allows providers to withhold separately maintained psychotherapy notes.
Valid denial grounds include:
- Clinically supported determinations of potential patient harm.
- Requests for psychotherapy notes are maintained separately from the general record.
Invalid denial grounds include:
- Administrative burden or staffing limits.
- Unpaid medical bills unrelated to copying costs.
- Vague privacy concerns that do not meet statutory criteria.
- Subpoenas submitted without required authorization or a qualifying court order.
Common deficiencies that lead to rejection include incomplete patient information, expired or unsigned authorizations, or missing HIPAA-required elements—particularly explicit consent for sensitive record categories.
Texas requires written denial notices within 15 days, including the basis for denial and information on review rights. Providers must also follow fee-notification rules—5 business days to issue a fee notice and 10 business days to receive payment under 22 TAC § 76.3.
Maintaining clear delivery proofs and complete authorization documentation supports timely follow-up and escalation to the Texas Medical Board or HHS Office for Civil Rights when necessary.
Texas Medical Board Escalation Process
The Texas Medical Board (TMB) regulates physicians and certain licensed health professionals but does not oversee hospitals, insurers, or HIPAA-specific privacy issues. Complaints must identify a TMB-licensed provider and cannot be submitted anonymously.
In medical-record disputes, TMB reviews whether a provider failed to release records as required under state or federal law. Outcomes include dismissal, corrective action, or referral for further review. Most matters resolve informally, and the Board generally conducts an initial jurisdictional evaluation within 45 days.
TMB complaint information and submission options are available through the My TMB Portal or by contacting the agency directly.
Improving Medical Record Retrieval Efficiency
Efficient medical record retrieval helps legal teams reduce delays created by manual requests, provider-specific procedures, and repeated follow-ups. Standardized authorizations, organized outreach, and clear deadline tracking give paralegals a more structured starting point and help firms obtain complete records before building chronologies or evaluating claims.
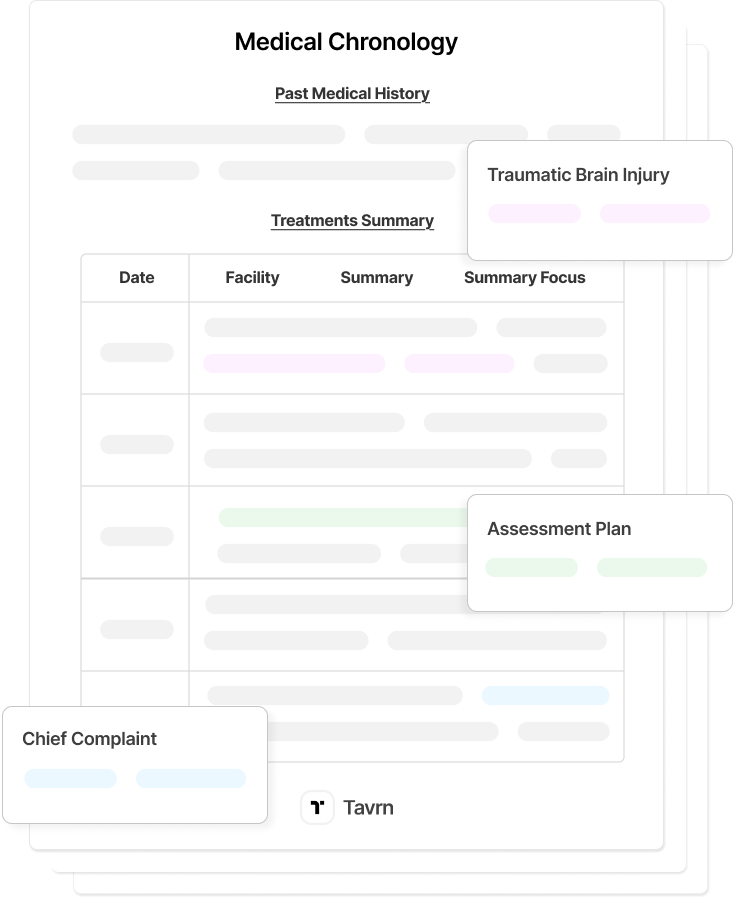
AI-powered retrieval tools, like Tavrn, reduce these delays by automating provider outreach, tracking responses, and consolidating released records into a single, review-ready set. Firms still verify completeness and maintain responsibility for HIPAA compliance, but automated retrieval shortens the time between initial request and substantive case work. Faster access to complete records supports earlier case evaluation, clearer documentation, and stronger downstream workflows.
Faster Medical Record Retrieval in Texas
Texas law and HIPAA establish clear rights of access, but timely medical record production depends on complete authorizations, accurate provider information, and adherence to fee-notification rules under 22 TAC § 76.3. Understanding these requirements—including Texas’s explicit authorization standards for sensitive record categories—helps ensure predictable responses from physicians, hospitals, and other providers.
Tavrn supports this process by managing compliant submissions, centralizing documentation, and coordinating delivery across multiple provider types governed by different Texas fee structures. With consistent turnaround times, legal teams can begin case evaluation earlier and maintain steady momentum throughout litigation.






.webp)
.webp)