Demand letters frame liability, establish damages, and set the tone for settlement negotiations long before litigation formally begins. While preparing demand letters is often treated as routine, their structure, timing, and evidentiary support materially influence whether insurers respond promptly, counter meaningfully, or delay evaluation altogether. This article consolidates proven tactics for improving demand letter outcomes into a single, actionable framework.
Why Demand Letters Fail
Several factors explain the wide variance in demand letter outcomes. Cases with unclear liability, incomplete medical records, or demands that exceed adjuster settlement authority consistently underperform. Documentation gaps invite challenges and reduced settlement offers. Demands structured beyond adjuster authority levels trigger multilevel approval processes that delay resolution.
Among these factors, medical record documentation quality most directly determines settlement value. Adjusters systematically evaluate records before authorizing settlement offers, applying four primary criteria: a proportionality assessment comparing costs to injury severity; causation verification establishing clear causal relationships; a completeness review checking for gaps and inconsistencies; and treatment continuity monitoring verifying ongoing treatment patterns. Deficiencies in any of these areas give adjusters justification to reduce settlement authority. Peer-reviewed research confirms these deficiencies "undermine the credibility of the medical record and weaken proof of causation or negligence."
The following eight tactics address these failure points: strengthening liability presentation, closing documentation gaps, aligning demand positioning with adjuster authority, and systematizing follow-up to maintain accountability.
1. Establish a Clear Liability Narrative
Effective demand letters establish liability through objective evidence rather than conclusory assertions. Police reports, witness statements, and expert opinions create a factual foundation adjusters can rely on when justifying settlement authority internally. Liability narratives that align facts with legal theories, while anticipating likely defenses, strengthen an adjuster's ability to recommend settlement approval.
The most effective liability presentations organize evidence sequentially, establishing duty, breach, causation, and damages through documentary support at each stage. This structure mirrors the analysis adjusters perform internally, reducing cognitive friction and accelerating evaluation.
2. Substantiate Economic and Non-Economic Damages
Successful demands present damages in a manner that is verifiable, organized, and consistent with insurer evaluation standards. Economic damages require corroboration through tax returns, employer verification letters, and itemized medical bills organized by provider and date of service. Non-economic damages benefit from structured framing; per diem approaches have been shown to increase non-economic damage awards when supported by medical evidence and functional limitations.
Economic damage documentation should include:
- Medical bill summaries organized by provider and date of service.
- Employer verification letters confirming lost wages and job performance impact.
- Tax returns establishing pre-injury earning capacity for comparison.
Incomplete or poorly organized damage documentation limits adjuster settlement authority regardless of injury severity. The challenge for many firms lies in extracting and organizing this information from hundreds of pages of medical records spread across multiple providers.
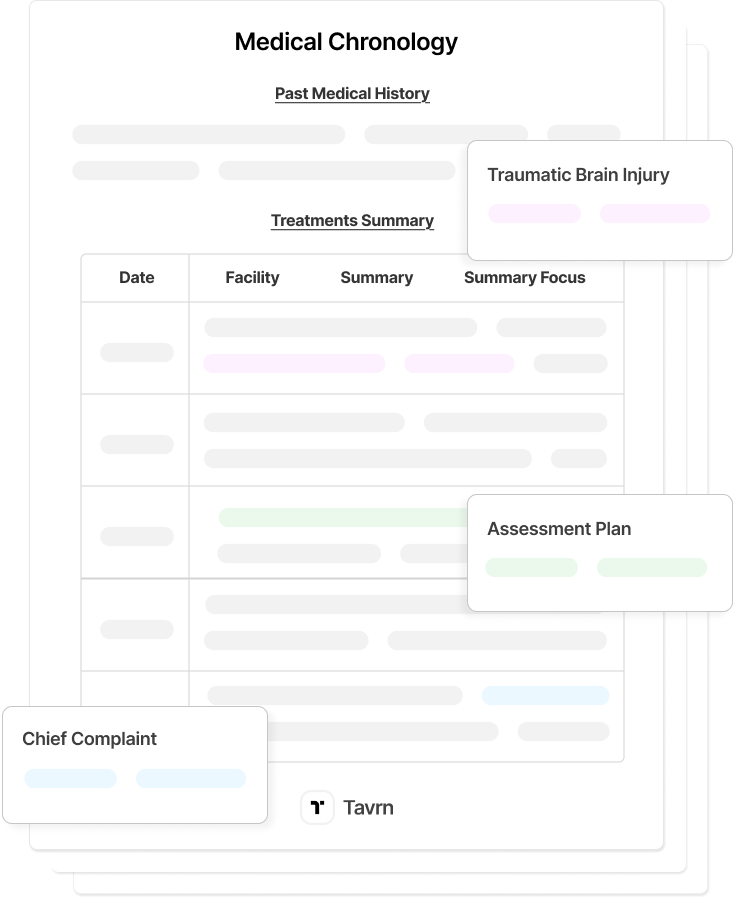
Tavrn's MedChron system addresses this organizational burden by transforming raw medical records into structured chronologies with automated extraction of diagnoses, treatments, and billing information. The platform's automated damages calculation pulls verified figures directly from organized records, ensuring economic damage presentations meet insurer verification standards without manual compilation errors.
3. Complete Medical Records Before Sending the Demand
Premature demands sent before treatment completion routinely result in incomplete documentation and depressed settlement values. The appropriate time to issue a demand letter is after the claimant reaches maximum medical improvement (MMI), when the condition has stabilized, and future medical needs become reasonably predictable.
Essential components of a complete demand package include:
- Itemized medical bills with treatment narratives and lost-wage verification.
- Pain and suffering documentation, including client diaries and functional limitation descriptions.
- Police reports, witness statements, and expert causation opinions.
- Future medical cost projections from treating physicians.
- Sequential photographic evidence documenting injury progression.
Sending demands 60–90 days after treatment completion ensures that adjusters have sufficient documentation to justify higher settlement authority. Settlement timelines depend heavily on injury severity and case complexity: minor injuries with clear liability typically resolve within several months after treatment completion, moderate injuries requiring ongoing treatment extend timelines as documentation develops, and serious injuries or disputed liability may take one to several years to resolve.
However, the documentation timeline often extends not because treatment continues, but because medical record retrieval from providers takes weeks or months. Manual provider outreach via fax and email, combined with follow-up delays and incomplete responses, creates bottlenecks that push demand timing well beyond optimal windows.
Automated medical record retrieval through Tavrn's nationwide provider network reduces retrieval timelines from weeks to days. One-click requests trigger system-managed provider follow-ups, with AI agents handling facility calls directly to eliminate hold times. Records arrive organized and tagged for efficient review, ensuring that documentation completeness—not administrative delays—determines when demands go out.
4. Align the Demand Amount with Documented Damages
Most insurers apply a multiplier methodology when valuing non-economic damages, applying a 1.5–5x factor to economic damages based on injury severity, liability clarity, and jurisdiction-specific norms.
Typical multiplier ranges include:
- 1.5–2x: Minor soft-tissue injuries with complete recovery.
- 2–3x: Moderate injuries requiring extended treatment.
- 3–4x: Serious injuries with permanent impairment.
- 4–5x: Severe or catastrophic injuries with lasting disability.
Demands that significantly exceed documented damages without evidentiary support are often categorized as adversarial, prompting extended evaluation timelines and aggressive counter-positions.
The key is ensuring damage calculations reflect complete, verified documentation rather than estimates based on incomplete records. Tavrn's demand letter preparation integrates directly with medical chronologies to calculate damages from verified treatment records. The platform automatically extracts billing totals, treatment costs, and documented functional limitations, enabling demand amounts that align precisely with the evidentiary record. This integration reduces the risk of demands that either undervalue cases due to missed documentation or overreach beyond what records support.
5. Leverage Nuclear Verdict Trends Strategically
Rising jury awards create external pressure that influences settlement posture. Adjusters evaluating trial risk consider recent verdicts within the jurisdiction, particularly cases involving similar injuries or liability theories. Demand letters that reference comparable local verdicts frame the financial risk of non-settlement and contextualize policy-limit exposure.
Jurisdictions with documented nuclear verdict trends—awards exceeding $10 million—provide additional leverage when policy limits are implicated. Citing specific verdicts demonstrates litigation awareness and signals preparedness to proceed to trial if settlement efforts fail. Effective verdict references include case name, jurisdiction, verdict amount, and injury similarity to the current matter.
The strategic value of verdict references depends on selecting comparable cases. Verdicts involving similar injury types, liability theories, and defendant categories carry more weight than large awards from dissimilar matters. Regional verdict databases and legal publications provide searchable access to recent outcomes that strengthen policy-limit positioning. When referencing verdicts, include sufficient detail to establish comparability: the injury mechanism, defendant type, liability theory, and verdict breakdown between economic and non-economic damages.
6. Set a Firm Response Deadline with Stated Consequences
Time-limited demands impose operational constraints on insurers. Setting response deadlines of two to four weeks, paired with clearly articulated consequences, creates internal urgency. Deadline language must specify concrete actions, such as filing suit, pursuing policy-limits litigation, or documenting unreasonable delay for potential bad-faith exposure.
California Code of Civil Procedure Section 999, effective January 1, 2023, formalizes requirements for time-limited policy-limit demands, including minimum response periods and documentation standards. Similar statutory and common-law frameworks in other jurisdictions reinforce the importance of precise deadline construction. Demands that lack specific deadlines or concrete consequences allow insurers to deprioritize evaluation without operational pressure.
Effective deadline provisions specify the exact date by which response is required, the form of acceptable response, and the specific actions that will follow non-response. Vague language like "prompt response requested" fails to create the operational urgency that drives timely evaluation.
7. Maintain a Professional Tone and Reasonable Positioning
Professional, objective language consistently produces better adjuster engagement than emotionally charged or adversarial demands. Excessive demands unsupported by documentation signal unrealistic expectations and frequently result in prolonged negotiations or outright rejection.
Positioning demands within or near adjuster settlement authority facilitates faster resolution. Less experienced adjusters typically have limited authority, while higher-value claims require escalation. Demands that exceed an adjuster's authority introduce additional scrutiny and delay, even when liability and damages are strong. Understanding typical authority thresholds—which vary by insurer and claim type—enables strategic positioning that avoids unnecessary escalation while maximizing recovery within efficient resolution timelines.
The tone of demand communications also affects ongoing negotiation dynamics. Adversarial language early in the process can poison subsequent discussions, while professional framing preserves the collaborative relationship needed for efficient resolution. Demands that present facts objectively and acknowledge legitimate questions about case value demonstrate confidence without aggression.
8. Follow Up Systematically When Insurers Do Not Respond
Structured follow-up reinforces accountability while building an evidentiary record. Consistent documentation of insurer delays strengthens negotiating leverage and supports extracontractual liability arguments if litigation becomes necessary.
Recommended follow-up timeline:
- Day 0: Send demand via certified mail with a 30-day response deadline.
- Day 7–10: Confirm receipt by phone and document with follow-up email.
- Day 30: Send written notice of missed deadline requesting status.
- Day 45+: Evaluate filing suit or documenting bad-faith delay.
Each communication should be documented with timestamps, recipient identification, and response content. This contemporaneous record becomes critical if bad-faith claims arise later in litigation. Follow-up communications should reference the original demand date, restate the deadline, and document the specific delay without inflammatory language that could undermine professional credibility.
Systematic follow-up also provides opportunity to supplement the original demand with additional documentation that becomes available, such as updated medical records, additional expert opinions, or new evidence supporting liability. Each supplement should reference the original demand and restate the response deadline.
How Tavrn Supports Demand Letter Success
The tactics above share a common thread: each depends on complete, organized documentation delivered within strategic timing windows. When record retrieval delays case preparation, or when damage calculations rely on manually compiled figures, even well-structured demands underperform.
Tavrn's platform connects these documentation requirements into a single workflow. The MedChron system identifies inconsistencies and treatment gaps that adjusters flag during evaluation, surfacing potential challenges before demands go out rather than after insurers raise objections. The demand letter preparation module preserves attorney oversight while eliminating the manual compilation that introduces errors and delays. Firms using this integrated approach report faster time-to-demand and documentation that anticipates adjuster evaluation criteria rather than reacting to it.
Building Stronger Pre-Litigation Results
Demand letter success improves when documentation is complete, medical narratives establish clear causation, and timing aligns with MMI. Understanding adjuster evaluation criteria and settlement authority structures enables strategic positioning that accelerates resolution by reducing multilevel approval requirements. Practitioners who systematize their approach to demand preparation, complete records, accurate damage calculations, and firm deadlines consistently achieve better pre-litigation outcomes.
Tavrn's integrated platform supports these outcomes through automated record retrieval that reduces preparation delays, streamlined medical record analysis that identifies documentation gaps, and AI-powered chronology generation that organizes treatment histories into coherent demand packages.






.webp)
.webp)