Medical chronologies serve as foundational documents in personal injury and medical malpractice litigation, shaping how attorneys, experts, and courts understand treatment timelines, causation, and the calculation of damages.
Errors in chronology preparation remain a recurring source of litigation risk: peer-reviewed research in PubMed Central estimates that 10–20% of medical malpractice lawsuits stem directly from documentation errors.
This article examines the nine most common medical chronology mistakes that weaken case narratives, explains why these errors occur in high-volume legal environments, and outlines evidence-based approaches for improving accuracy, quality control, and defensibility in chronology preparation.
Why Do Medical Chronology Errors Matter?
Errors in medical chronologies carry direct litigation consequences because chronologies shape how attorneys, experts, and courts interpret causation, damages, and treatment timelines. Bar guidance emphasizes that chronologies must extract and present discrete, verifiable medical facts rather than merely listing records; failures in accuracy or structure undermine that function.
The downstream effects are significant:
- Settlement impact: Inaccurate or incomplete chronologies weaken injury narratives and causation theories, reducing negotiation leverage during pre-suit and mediation phases.
- Case dismissal risk: Courts have imposed terminating sanctions where medical evidence was misstated, omitted, or improperly produced during discovery.
- Professional liability exposure: Chronology errors that contribute to missed deadlines, evidentiary exclusions, or adverse rulings can form the basis of legal-malpractice claims against counsel.
In short, chronology accuracy is not clerical—it directly affects evidentiary reliability, procedural compliance, and case valuation.
How These Mistakes Affect Legal Outcomes
According to peer-reviewed research, physicians win 80-90% of cases where evidence of negligence is weak, but only 50% of cases with strong evidence. Chronology errors that misrepresent critical events can shift cases between evidence quality categories, altering win probabilities by 20-40 percentage points.
Chronology errors directly undermine negotiation leverage by creating confusion and weakening causation narratives. Research demonstrates that accurate chronologies correlate with 26-40% settlement increases, while errors can result in case dismissal or $1 million+ liability findings.
Why Do Medical Chronology Errors Happen?
Medical chronology errors emerge from structural operational factors rather than individual performance failures.
Role Complexity and Attention Fragmentation
According to the ABA paralegal negligence analysis, paralegals must manage medical records "spanning years or even decades, often involving multiple healthcare entities" while simultaneously handling legal research, trial preparation, and coordination across multiple parties. This multi-dimensional workload creates attention fragmentation, increasing the probability of errors.
Volume Pressures and Time Constraints
High-volume personal injury practices often manage dozens of active cases simultaneously, with paralegals juggling record requests, chronology preparation, and filing deadlines across multiple matters.
The compressed timeframes between receiving medical records and discovery deadlines leave insufficient time for thorough review. Additionally, the exponential growth of medical records driven by electronic health record systems means a single hospital stay can generate hundreds of pages of documentation, multiplying the opportunity for errors.
Specialization Gap
The American Bar Association recommends that firms employ "nurse paralegals with medical knowledge" for medical record review. This recommendation reveals that standard paralegal training may be structurally insufficient for accurate medical chronology work.
Without clinical training, paralegals lack foundational knowledge to interpret complex medical terminology, recognize clinically significant events, and understand temporal relationships between treatments and outcomes.
The 9 Most Common Medical Chronology Mistakes
Medical chronologies are critical to establishing treatment timelines, causation, and damages. The following sections identify the most common medical chronology mistakes that weaken case narratives and create vulnerabilities in liability and settlement analysis.
1. Incomplete Medical Record Collection
Failing to obtain all relevant medical records is the most fundamental chronology error. Comprehensive collections extend beyond hospital charts and physician notes to include imaging, laboratory data, prescription histories, and records from every treating provider.
Commonly missed sources include pharmacy dispensing logs, physical therapy and rehabilitation records, emergency medical services (ambulance) reports, mental health treatment files, and workers’ compensation medical evaluations. For example, omitting pharmacy records can obscure medication adherence or dosage changes that become central to causation or damages disputes.
2. Organizational and Structural Failures
Chronologies that lack consistent structure or contain disordered dates undermine usability and credibility. Bar guidance cautions against chronologies that merely mirror document order instead of presenting extracted medical facts in a coherent timeline.
For example, mixing narrative summaries with raw document references without a standardized format forces attorneys and experts to re-interpret the chronology, increasing the risk of missed events or misstatements during testimony.
3. Medical Terminology Errors
Misinterpreting medical abbreviations or using inconsistent terminology introduces factual inaccuracies that can materially alter case narratives. Even minor terminology errors can misrepresent treatment intensity, symptom severity, or patient compliance.
Common examples include confusing “QD” (once daily) with “QID” (four times daily), misreading “C/O” as “care of” rather than “complains of,” or treating “PT” as “patient” instead of “physical therapy.” A single dosing error in a chronology can misstate medication exposure and affect both liability and damages analysis.
4. Omission of Critical Medical Events
Rushed or superficial review often results in missing pivotal clinical events that directly affect causation or standard-of-care analysis. These omissions may involve changes in treatment plans, complications, or deviations from expected care.
For example, in Brown v. St. Clair Anesthesia, Ltd., the failure to document a catheter type change became central to liability findings, contributing to a $1 million outcome. Similar omissions can distort expert opinions and weaken trial narratives.
5. Date Sequencing Failures
Assuming records arrive in the correct chronological order without independent verification leads to inaccurate timelines. Medical records frequently arrive out of sequence due to batching, late production, or EHR export limitations.
For instance, placing diagnostic imaging before the emergency department visit that prompted it may incorrectly suggest a pre-existing condition. Likewise, misplacing referral dates relative to surgery can undermine arguments about informed consent or care coordination.
6. Source Document Traceability Failures
Chronology entries that lack clear references to source documents, page numbers, or Bates ranges reduce defensibility. Courts and experts expect each factual assertion to be traceable to underlying records.
For example, noting a diagnosis or complication without citing the originating progress note or operative report makes it difficult to verify accuracy during deposition or cross-examination, increasing evidentiary risk.
7. Electronic Health Record Interpretation Failures
Electronic health records organize and timestamp data differently from paper charts. Timestamps may reflect data entry rather than event occurrence, and copy-forward features can duplicate outdated information across encounters.
A common example is relying on auto-populated medication lists without verifying actual administration dates, which can result in chronologies reflecting treatments that were discontinued or never given.
8. Failure to Identify Documentation Inconsistencies
Chronologies that simply summarize records without analyzing contradictions fail to add analytical value. Inconsistencies between provider notes, gaps in treatment, or conflicting diagnoses often signal issues requiring follow-up.
For example, differing accounts of symptom onset across emergency and follow-up visits may affect causation opinions. Failing to flag these discrepancies leaves attorneys and experts unaware of potential challenges.
9. Case Narrative Failures
Document-focused chronologies that list encounters without connecting medical events to liability theories weaken case strategy. Effective chronologies synthesize facts into narratives that explain how care decisions led to injury and damage.
For example, listing postoperative complications without linking them to alleged deviations from the standard of care provides limited strategic value. Narrative-driven chronologies better support expert testimony, jury comprehension, and settlement negotiations.
Narrative-focused chronologies are commonly used to present medical events in a form that experts, courts, and factfinders can evaluate efficiently, particularly where causation and damages depend on temporal relationships.
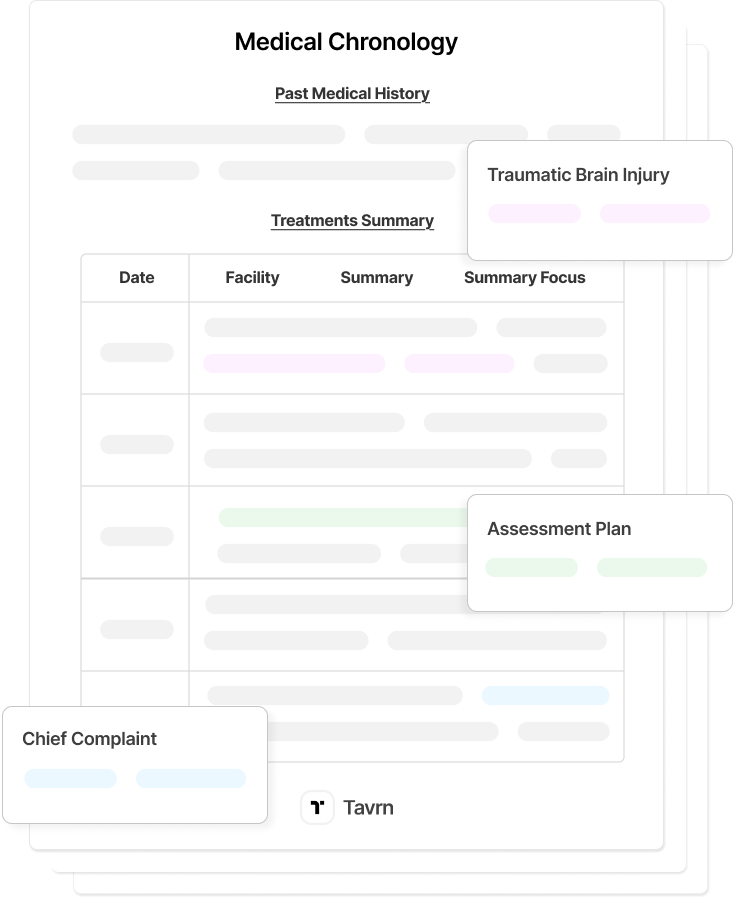
How AI-Powered Chronology Tools Reduce Errors at Scale
AI-powered medical chronology tools reduce error rates by enforcing structured review workflows, source verification, and consistency controls that are difficult to sustain in manual, high-volume environments. Rather than relying on single-pass summarization, these systems apply multi-stage processing that reflects quality-control practices used in complex litigation and large medical-record productions.
In practice, AI-assisted chronologies address the most common error categories as follows:
- Incomplete record collection: Pattern analysis across facilities and treatment periods surfaces missing providers, unexplained gaps, and incomplete date ranges during medical record retrieval, before chronology construction begins.
- Organizational and sequencing failures: Automated ordering by verified encounter dates corrects out-of-sequence production and EHR export issues, producing clearer, defensible medical chronologies.
- Terminology and interpretation errors: Standardized clinical vocabularies reduce misinterpretation of abbreviations and shorthand, while flagging ambiguous entries for human review during medical record review.
- Omitted critical events: Event-detection models identify diagnoses, procedures, medication changes, and complications that may be missed in manual review of large record sets.
- Source document traceability failures: Chronology entries retain direct links to source documents and page references, preserving evidentiary reliability during discovery and expert analysis.
- EHR-specific pitfalls: Systems distinguish documentation timestamps from actual event times, limiting errors caused by copy-forward notes and delayed data entry.
- Unidentified documentation inconsistencies: Cross-record comparison reveals conflicting provider notes, duplicated information, and internal contradictions that require further review.
Maintaining accuracy at scale requires more than automation alone. Law firms typically rely on one of three models: outsourcing chronologies to specialized vendors, implementing in-house AI systems, or using hybrid approaches that combine internal oversight with AI-assisted processing. Platforms such as Tavrn are designed to support all three models by standardizing chronology structure, source linking, and review checkpoints regardless of where final validation occurs.
Firms that maintain quality across growing case volumes consistently track a limited set of indicators, including chronological clarity, error rates identified during secondary review, attorney time spent correcting timelines, and downstream effects on case evaluation. By reducing structural and clerical errors upstream, AI-assisted chronologies allow legal teams to focus on substantive analysis rather than reconstructing timelines from disorganized records.
Manual vs. Scaled Approaches to Chronology Accuracy
According to a 2024 PubMed Central study, manual patient chart review takes up to 30 minutes per patient and achieves 93.8% initial accuracy—but 36.6% of manual reviews require corrections upon a second review.
According to IDC research, document review represents the primary use case for generative AI adoption, with 65% of legal organizations planning implementation within one year. The Federal Bar Association's 2025 Report shows personal injury lawyers among leading AI adopters, with 37% reporting personal use and 20% reporting firm-wide implementation.
The cost implications are substantial: manual approaches require significant paralegal hours per case, while scaled approaches reduce per-case costs by 50-80%.
Error rates in manual processes average one-in-three reviews requiring correction, compared to technology-assisted approaches that flag inconsistencies automatically. Time-to-completion differences are equally dramatic, with manual chronologies taking days compared to hours for scaled solutions.
Maintaining High Accuracy Standards at Scale
For firms considering medical chronology outsourcing, specialized vendors offer access to medical-legal experts without permanent hiring. Law firms employ three primary approaches: outsourcing to specialized vendors, implementing in-house AI solutions, and using hybrid models combining internal resources with selective outsourcing.
Firms maintaining quality at scale track specific KPIs: chronological clarity, error rates found during review, attorney time savings, and settlement outcome impact.
Reduce Chronology Mistakes with Tavrn
Medical chronology errors stem from structural challenges, including role complexity, specialization gaps, and inadequate quality control. Implementing multi-stage verification processes, engaging clinical expertise, and leveraging technology with human oversight can significantly reduce error rates.
Available service options provide multiple pathways to address accuracy challenges through source-linked verification and litigation-ready outputs delivered within hours.





.webp)
.webp)