Paralegals managing 25-40 active cases already know how medical record retrieval works. The problem isn't the process; it's that even perfect execution still means weeks of waiting while cases sit idle and attorneys ask for updates.
Understanding how to request medical records from a hospital efficiently requires mastery of the HIPAA Privacy Rule's right of access under 45 CFR § 164.524 and compliant authorization requirements per 45 CFR § 164.508. The process involves identifying correct hospital departments, completing HIPAA-compliant authorizations, and navigating fee structures that vary by state and request type.
This guide covers HIPAA access rights, step-by-step request procedures, fee limitations, litigation-specific requirements, and resolution strategies. Legal professionals handling case preparation workflows will find actionable frameworks for streamlining record retrieval.
HIPAA Rights for Hospital Medical Record Requests
The HIPAA Privacy Rule establishes foundational access rights under 45 CFR § 164.524. Hospitals must provide access to protected health information within 30 calendar days, with one permitted 30-day extension requiring written notice.
Records Subject to Access Rights
The "designated record set" defined in 45 CFR § 164.501 includes medical records, billing records, case management records, and electronic health records used for treatment or billing decisions.
Psychotherapy Notes Exception
Psychotherapy notes receive special protection when separated from the general medical record. However, HHS guidance clarifies that medication prescriptions, session timing, treatment modalities, clinical test results, and diagnosis summaries must be disclosed upon valid request.
Right to Amend Records
Under 45 CFR § 164.526, patients have the right to request amendments to their medical records. Hospitals must respond within 60 days, with one permitted 30-day extension. Patients who disagree with denials may submit a statement of disagreement that must accompany the disputed information in all future disclosures.
How to Request Hospital Medical Records: Step-by-Step
Medical record requests fail most often due to incomplete submissions or misdirected correspondence, not complex legal issues. A systematic approach ensures requests reach the correct department with all required elements, reducing rejection rates and accelerating response timelines.
Identify the Right Department
Contact the hospital's main line and request transfer to "Health Information Management," "Medical Records," or "Release of Information"—terminology varies by facility. Large health systems may route requests through centralized processing centers rather than individual hospital locations.
Document the department name, direct phone number, and fax number. Verify the correct submission address before sending—misdirected requests restart the 30-day timeline.
Complete the Authorization Form
45 CFR §164.508(c) requires these mandatory elements:
- Specific description of information requested with date ranges
- Name of disclosing entity (hospital's complete legal name)
- Name of authorized recipient (law firm and specific attorney/paralegal)
- Purpose of disclosure ("legal representation" or "litigation")
- Expiration date or event
- Patient signature and date
- Statement regarding right to revoke
- Redisclosure warning
- Non-conditioning statement
Submit the Request
Submit via certified mail with return receipt or fax with transmission confirmation. Include the completed authorization, cover letter, specific records requested with date ranges, and contact information. Address submissions to the HIM or ROI department at the specific hospital location where treatment occurred.
The cover letter should identify the patient by name, date of birth, and medical record number if known. Specify exact record types needed — "all records" invites partial production. Include a return deadline referencing HIPAA's 30-day requirement and provide both fax and email for delivery options. Retain copies of everything submitted.
Track and Follow Up
The 30-day HIPAA timeline begins upon hospital receipt—but providers routinely treat it as a suggestion rather than a requirement. Systematic follow-up prevents requests from stalling indefinitely.
Escalation framework:
- Day 7-10: Call HIM to confirm receipt and obtain a reference number. Document the representative's name.
- Day 14: If no acknowledgment, send written follow-up via fax with delivery confirmation. Reference the original submission date and request status update.
- Day 25: Call HIM again. If records remain "in the queue," request supervisor contact information and anticipated completion date.
- Day 30: Send formal letter citing 45 CFR § 164.524(b)(2), noting that the response deadline has passed and requesting immediate processing.
- Day 45: If no response or extension notice, escalate to the hospital Privacy Officer. Reference potential OCR complaint.
- Day 60: File OCR complaint through the HHS portal if records remain outstanding.
Maintain a tracking log documenting every contact attempt, representative name, and stated timeline. This documentation supports OCR complaints and demonstrates good-faith efforts if litigation over access becomes necessary.
Partial production is common. When records arrive incomplete—missing radiology, nursing notes, or billing—send a supplemental request immediately, identifying specific gaps with date ranges.
Hospital Medical Record Request Methods
Submission method affects both turnaround time and record completeness. Patient portals offer speed but limited scope; written requests provide comprehensive production with authentication-ready documentation.
Patient portals may provide preliminary access to recent treatment notes but feature fragmented access and incomplete historical records. For litigation purposes, mail/fax requests with proper HIPAA authorization remain the established standard, providing documentary evidence and authentication-ready certifications.
Written requests provide clear paper trails with authentication-ready documentation. Per AHIMA professional standards, hospitals can provide certified copies with business record affidavits when specifically requested for trial use. Reserve in-person requests for high-stakes cases approaching trial deadlines.
Medical Record Request Fees and State Timelines
HIPAA's fee limitations under 45 CFR § 164.524(c)(4) apply only to patient-initiated requests, limited to labor for copying, supplies, and postage. The regulation permits a flat fee not exceeding $6.50 for electronic copies.
Third-Party Legal Requests Differ
Attorney-requested records fall under state law fee schedules. The Texas Health and Human Services fee schedule permits charges substantially exceeding HIPAA limits, including page fees ranging from $0.54-$2.03 per page plus retrieval fees up to $108.89.
State Timeline Variations
- California: 15 calendar days.
- Texas: 15 business days.
- New York: 10 days for inspection, 20 days for copies.
- Florida: 14 calendar days.
Hospitals must comply with state timelines when shorter than federal requirements.
Requesting Hospital Medical Records for Litigation
Litigation requests involve additional complexity beyond standard patient access rights. Third-party authorization requirements, specially protected record categories, and alternative pathways like subpoenas each carry distinct procedural requirements, and common rejection points that delay case preparation.
Third-Party Authorization Requirements
45 CFR 164.512(e)(1)(ii) requires "satisfactory assurances" demonstrating either patient notice or a qualified protective order. Common authorization rejection reasons include missing required HIPAA elements, vague record descriptions, failure to obtain separate authorizations for specially protected records, and use of outdated authorization forms.
Which Records to Request for Legal Cases
Standard requests often miss records that prove critical during discovery or expert review. Build requests around comprehensive production, not minimum documentation.
Critical records include operative reports and anesthesia records, discharge summaries, nursing documentation and shift reports, radiology images AND interpretation reports, itemized billing records with procedure codes, and incident reports (may require subpoena). Commonly overlooked records include pharmacy dispensing records, EMR audit trails, and nursing shift handoff notes.
Subpoenas and Court Orders
When patient authorization is unavailable, 45 CFR 164.512(e) permits three pathways: court orders signed by a judge, subpoenas with patient notice and satisfactory assurances, and subpoenas accompanied by qualified protective orders.
A qualified protective order must prohibit parties from using or disclosing PHI for any purpose other than the specific litigation and require the return or destruction of all PHI copies at the conclusion of litigation. This pathway is particularly useful when building comprehensive medical chronologies for case preparation.
Common Medical Record Request Obstacles
Even properly submitted requests encounter resistance. Non-responsive providers, inflated fee demands, and incomplete production are routine, not exceptions. Knowing the regulatory leverage points and escalation pathways turns weeks of follow-up into documented pressure that compels compliance.
Non-Response Beyond 30-Day Deadline
Silence is the most common obstacle. Providers frequently ignore initial requests, betting that requestors won't follow up with regulatory teeth.
At day 31, send a formal letter citing 45 CFR § 164.524(b)(2) and stating the facility is now in violation of federal access requirements. If no response by day 45, escalate to the hospital's Privacy Officer, not HIM. At day 60, file an OCR complaint through the HHS complaint portal. Recent enforcement actions have resulted in penalties of $70,000 to $200,000 for access violations; mentioning this history in correspondence often accelerates response.
Excessive Fees
Fee disputes require state-specific analysis. Providers frequently quote amounts exceeding statutory limits, particularly for third-party legal requests where they assume requestors won't challenge.
Request an itemized invoice before paying and compare against applicable state fee schedules. For patient-initiated requests, cite HHS prohibition on charging more than reasonable cost-based fees. The $6.50 flat fee option applies only to individual access requests, not third-party legal requests — know which standard applies before disputing.
Incomplete Records
Partial production is standard practice, not an anomaly. Providers frequently omit radiology images (sending only interpretation reports), nursing notes, pharmacy dispensing logs, or billing records.
Before accepting any production as complete, cross-reference received records against the patient's treatment narrative. Send supplemental requests within 10 days specifying exact gaps: "Radiology images from CT scan performed 3/15/2024 were not included. Please provide images in addition to the interpretation report already received."
Building Reliable Retrieval Workflows
Effective medical record retrieval requires mastery of HIPAA authorization requirements, strategic method selection, and systematic follow-up protocols. Firms that systematize these workflows report 10-15 day average retrieval cycles compared to 30-45 days with manual processes, efficiency that directly impacts case capacity. State law variations add complexity, particularly regarding timelines and fee structures for third-party legal requests.
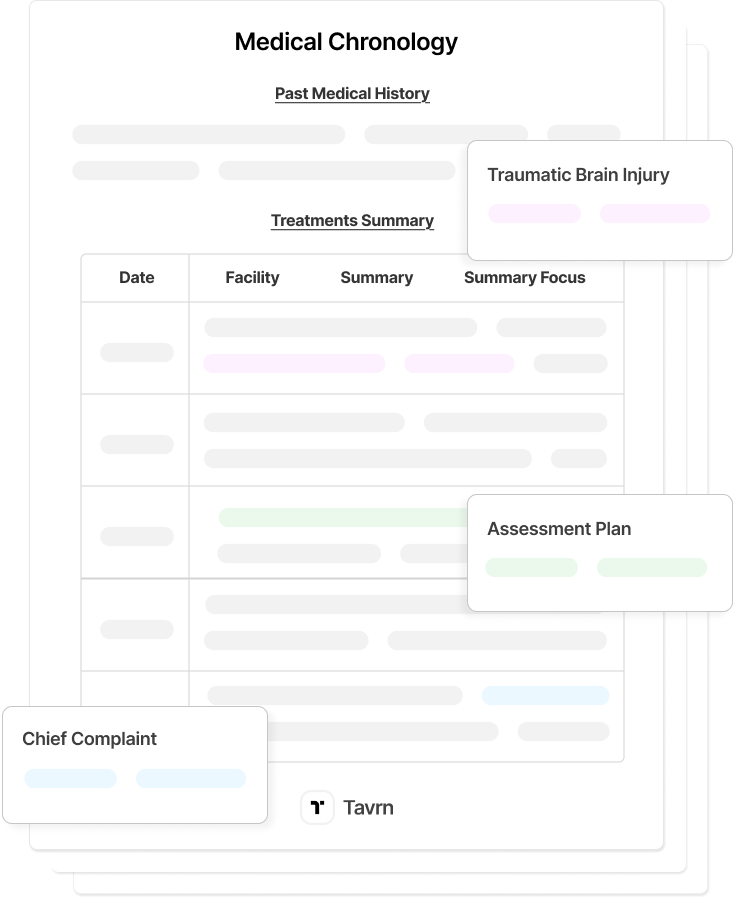
Tavrn automates the retrieval workflow—request submission, deadline tracking, provider follow-up—so paralegals can focus on the medical record analysis that actually requires their expertise.
Request a demo to see how Tavrn streamlines medical record retrieval for litigation.







.webp)
.webp)