Settlement day should mark the end of a case, not the beginning of a disbursement nightmare. Yet without systematic lien identification procedures implemented during record retrieval, paralegals managing personal injury caseloads risk discovering undisclosed liens during final accounting, which forces delays that frustrate clients and create malpractice exposure.
A lien in a personal injury case is a legal claim against settlement proceeds by a third party who paid for medical treatment or other services related to the injury. These claims must be satisfied before the client receives their net recovery.
This article examines the types of liens that attach to personal injury settlements, how lien priority affects case preparation, and the procedural requirements for identification and resolution.
What Is a Lien in a Personal Injury Case?
A lien creates a security interest in settlement proceeds, granting the lienholder a legal right to recover funds paid on behalf of the injured party. Unlike general creditors, lienholders have statutory or contractual authority to intercept settlement funds before distribution to the client.
Failure to identify and resolve liens before disbursement can result in double damages liability, civil monetary penalties up to $365,000 per instance, professional liability exposure, and depleted client recovery.
Liens attach through three primary mechanisms.
- Statutory liens attach by operation of law, including Medicare and Medicaid liens under federal statute, hospital liens under state statute, and workers' compensation subrogation rights.
- Contractual liens arise from agreements between the injured party and healthcare providers or insurers, including Letters of Protection.
- Attorney charging liens attach to judgment or settlement proceeds upon proper filing with the court clerk.
Types of Liens in Personal Injury Cases
Different lienholders derive their claims from different legal sources: some statutory, some contractual, some arising from federal law with preemptive authority over state protections. Identifying lien type determines available negotiation strategies, applicable defenses, and ultimate recovery limitations.
Healthcare Provider Liens
Healthcare provider liens operate through statutory frameworks that vary dramatically by state. California's hospital lien statute caps recovery at 50% of money due to the injured person after paying prior liens. Texas imposes a strict 72-hour admission requirement and a triple limitation formula applying the lesser of the first 100 days of hospitalization charges, 50% of amounts recovered, or the amount awarded, less pro rata attorney fees.
Letters of Protection create contractual claims carrying significant client financial risk. KFF Health News documents that providers routinely charge 200-300% higher rates under LOPs than standard insurance reimbursement.
Statutory lien perfection requires strict procedural compliance, including proper filing with court clerks, certified mail service to all parties, and adherence to state-specific deadlines. The Nevada Bar Association documents cases where hospitals lost substantial lien rights by serving notice one day after settlement payment.
Health Insurance and ERISA Liens
Under US Airways, Inc. v. McCutchen, plan language supremacy governs all ERISA subrogation disputes—equitable doctrines cannot override clear, unambiguous plan terms. However, if plan language is silent or ambiguous, courts may apply traditional equitable principles such as the common fund doctrine.
The critical threshold determination is whether the plan is fully-insured or self-funded.
- Fully-insured plans purchase coverage from a licensed insurance carrier and remain subject to state insurance regulation through ERISA's "savings clause," meaning state-law protections, including made-whole doctrines, often limit recovery rights.
- Self-funded ERISA plans have employers directly assume financial responsibility for claims, benefiting from federal preemption under ERISA Section 514(a), which supersedes state laws and eliminates state anti-subrogation statute protections.
Modern sophisticated ERISA plans routinely include explicit contractual language rejecting equitable doctrines regardless of funding structure.
Identification requires reviewing Summary Plan Descriptions, examining EOBs for funding structure indicators, and verifying through Department of Labor Form 5500 filings when plan documents are unavailable.
Government Liens: Medicare, Medicaid, and VA
Medicare's conditional payment system creates procedurally complex requirements. The Benefits Coordination & Recovery Center issues Conditional Payment Letters, and attorneys must respond within specified timeframes to dispute unrelated charges. Civil monetary penalties under 45 CFR Part 102 reach $365,000 per instance for non-compliance with reporting requirements or untimely reimbursement.
Medicaid liens are limited by the Ahlborn allocation framework, restricting recovery to the portion of settlement specifically allocated to past medical expenses.
This Ahlborn limitation does not apply to Medicare liens, which maintain full recovery rights against the entire settlement amount regardless of how proceeds are allocated between medical expenses and other damages.
VA healthcare liens operate under the Federal Medical Care Recovery Act (42 U.S.C. § 2651), granting independent federal recovery authority extending to both past and future medical care reasonably expected to be furnished.
Workers' Compensation Liens
Workers' compensation subrogation rights depend on the Made Whole versus first-money jurisdictional distinction. Made Whole states like Montana and Georgia require full employee compensation before carrier recovery. First-money states like Illinois permit carrier recovery regardless of complete compensation.
State-specific formulas create different lien reduction methodologies. Florida's Manfredo Formula significantly reduces lien recovery by accounting for the difference between settlement amount and total case value:
Manfredo Formula = Lien Amount × [(Settlement - Attorney Fees - Costs) / Full Case Value]
Early identification of workers' compensation liens is essential because carriers often monitor claims and may intervene in third-party litigation. Some jurisdictions require carriers to contribute proportionately to attorney fees under the common fund doctrine, while others allow full recovery without fee offset.
Attorney Liens
Charging liens attach to settlement proceeds in the specific case where services were rendered, requiring a contract between attorney and client, an understanding that fees come from recovery, dispute or avoidance of payment, and timely notice. Retaining liens provide possessory rights over client property until fees are paid, though California prohibits retaining liens per California State Bar Formal Opinion No. 2006-170.
Successor counsel must disclose settlements to prior counsel holding valid liens, even against client instructions, to protect valid lien interests.
Settlement funds containing third-party lien amounts must be deposited into the attorney's client trust account immediately upon receipt. The attorney has fiduciary obligations under ABA Model Rule 1.15 to hold third-party funds separately, promptly notify all lienholders, and promptly deliver funds to entitled parties.
Lien Priority in Personal Injury Settlements
Medicare maintains automatic statutory priority under the Medicare Secondary Payer provisions. Medicaid occupies second position as "payer of last resort," with recovery strictly limited by the Ahlborn allocation framework.
The practical hierarchy for settlement disbursement:
- Attorney charging liens
- Medicare conditional payments
- Medicaid liens
- Statutory hospital liens
- ERISA plan subrogation
- Workers' compensation liens
- Contractual provider liens and letters of protection
Not all liens carry equal weight in the disbursement hierarchy. Understanding priority determines which lienholders receive full payment, which receive partial payment, and which may be left with reduced or uncollectible amounts when settlement funds are insufficient to satisfy all claims.
Medicare's mandatory priority means its conditional payment claims must be satisfied before most other lienholders receive payment, potentially leaving subordinate lienholders with reduced amounts. When multiple liens compete for limited settlement funds, paralegals must calculate whether full satisfaction is possible or whether pro rata distribution becomes necessary. Accurate priority analysis early in case development prevents disbursement disputes and client dissatisfaction at settlement.
Why Medical Records Matter for Lien Identification
Medical records serve as the primary investigative tool for discovering lienholders. Systematic record organization prevents the costly mistake of discovering liens only after settlement negotiation begins.
Common documentation gaps that create lien identification failures include:
- Vague provider identifiers listing "clinic" without complete facility information.
- Missing itemized statements showing third-party payor sources.
- Treatment chronology gaps concealing facility transfers or episodic care.
- Absent referral notation failing to identify specialist involvement.
- Insurance coverage omissions include missing Medicare, Medicaid, or group health plan involvement.
Key documents include itemized medical bills containing payor fields, Explanation of Benefits showing which carriers processed claims, face sheets listing insurance coverage, and signed lien agreements, which some providers require at intake.
Medicare identification requires determining beneficiary status through EOB examination showing Medicare processing or Medicare ID numbers on billing statements. Medicaid indicators include state-specific program names and extremely low patient co-pays. Organized medical chronologies surface all providers systematically rather than relying on client memory or piecemeal record requests.
Negotiating and Resolving Personal Injury Liens
Effective lien negotiation deploys multiple strategies simultaneously. For Medicare, attorneys can dispute unrelated charges, file appeals for conditional payment errors, request financial hardship waivers through Form SSA-632-BK, or negotiate compromise under "best interest of the program" authority.
ERISA negotiation approaches include challenging plan language ambiguity, asserting equitable defenses, invoking the Common Fund Doctrine for proportionate attorney fee sharing, and disputing relatedness of medical charges. Plans drafted before McCutchen (2013) often lack explicit waivers, preserving made-whole and common fund arguments even for self-funded plans.
The Common Fund Doctrine requires lienholders who benefit from a settlement to contribute proportionately to the attorney fees and costs that created that fund, potentially reducing net lien amounts by 25-40%.
Hospital liens must strictly comply with statutory requirements regarding timing, notice, and recording. Non-compliance can invalidate the lien entirely—verification of procedural compliance should precede any negotiation. Common defects include:
- Late filing beyond statutory deadlines.
- Improper service or failure to serve all required parties.
- Missing statutorily required information, such as itemized charges or treatment dates.
Negotiation leverage varies dramatically by timing. Maximum leverage exists before settlement execution; minimal leverage remains after fund distribution.
Lien Identification Through Systematic Case Preparation
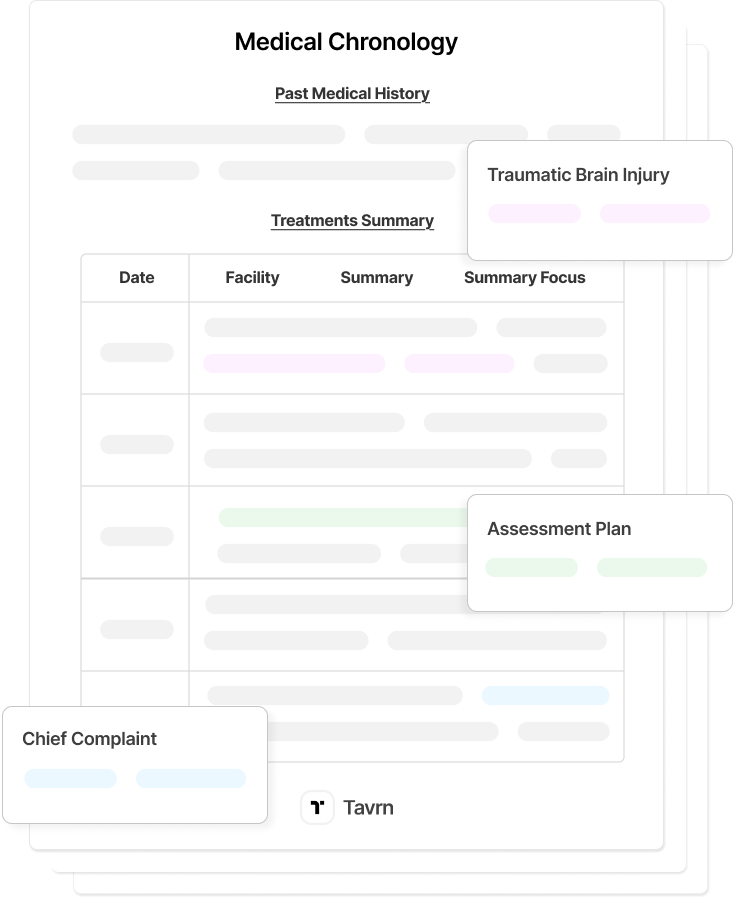
Comprehensive lien management requires structured medical chronologies and chronological documentation that reveals payment sources, treatment timelines, and insurance relationships. Paralegals who implement systematic lien identification at case intake—rather than scrambling during disbursement—protect their firms from liability exposure while ensuring clients receive accurate net recovery projections from the start.
Tavrn's AI-powered medical chronology and document processing capabilities create the organized foundation necessary for systematic lien identification. Automated medical record retrieval, indexing, and classification enable paralegals to more efficiently review documentation during the critical initial case assessment phase.







.webp)
.webp)